PICC常见并发症及其处理
2017-10-27 Ryy 肿瘤资讯
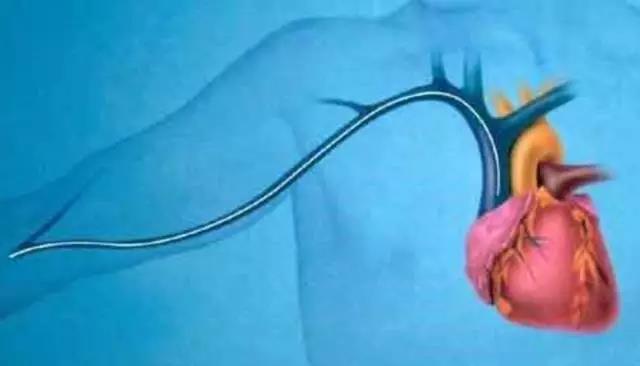
反复扎针很痛苦,PICC来帮忙。对于需要长期输液或输注高危液体的患者,PICC以其穿刺成功率高、可长期带管、减少外周静脉损伤等优势得到了广大患者及医务工作者的认可。但随着其临床应用的增多,并发症的出现也随之增加。那么,PICC常见的并发症有哪些?临床应该如何预防及处理呢?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#并发#
42
学习一下谢谢分享
83
#PICC#
53
#ICC#
46
学习了很多先进的医疗技术
72
学习了谢谢分享!!
57
谢谢分享.学习了
72
好资料学习了!
70
我们都值锁骨下静脉
34