Cancer Cell:中国癌症研究进展
2011-12-05 MedSci原创 MedSci原创
“中国是最大的发展中国家,经历了快速的工业化,城市化,和市场经济化。这些社会变革导致了一些不良后果,比如生态恶化,环境污染,这些都是癌症的诱发因素。除此之外,我们还有大约3亿的烟民,超过9千万的乙肝患者……” ——陈竺 著名癌症研究国际期刊Cancer Cell杂志最新推出了一份增刊:Spotlight on China,主要聚焦于中国目前癌症研究和治疗方面的进展,并介绍了国
“中国是最大的发展中国家,经历了快速的工业化,城市化,和市场经济化。这些社会变革导致了一些不良后果,比如生态恶化,环境污染,这些都是癌症的诱发因素。除此之外,我们还有大约3亿的烟民,超过9千万的乙肝患者……”
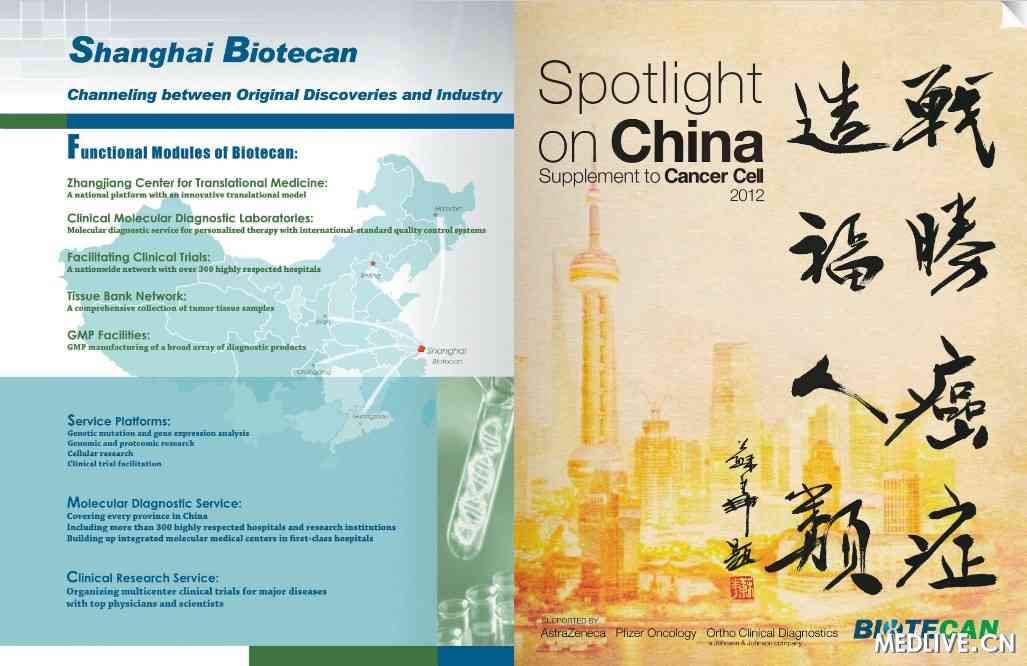
(Cancer Cell增刊封面,由苏华教授(音译)题字)
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Cell#
29
#CEL#
37
#cancer cell#
37
#研究进展#
35
#癌症研究#
0