JNCI:BRCA突变携带者行预防性输卵管卵巢切除术后,子宫内膜浆液性癌的发病风险降低了吗?
2017-08-26 佚名 肿瘤资讯
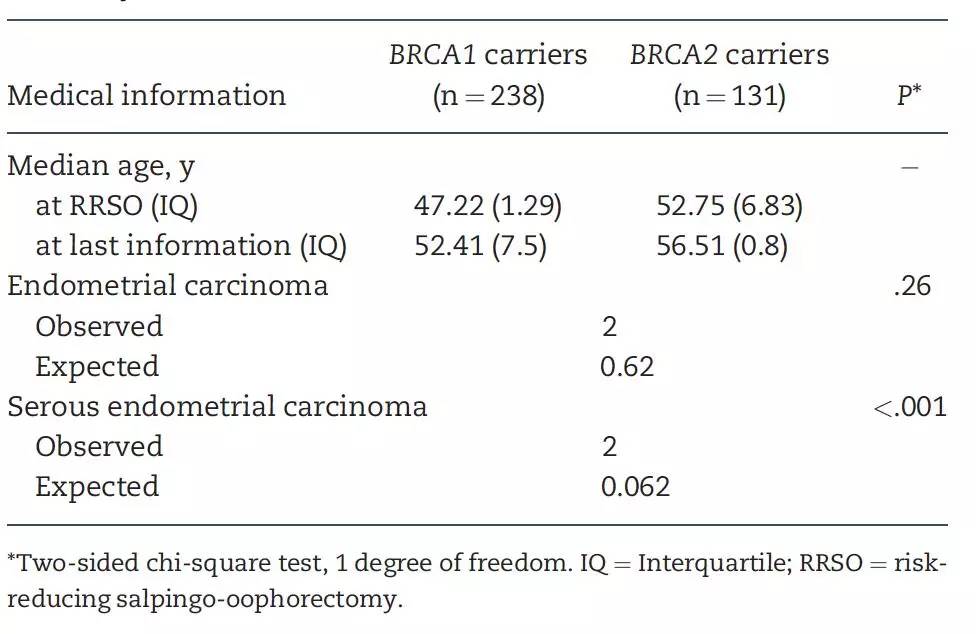
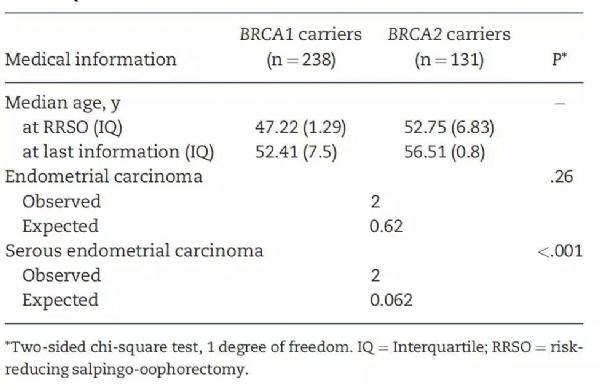
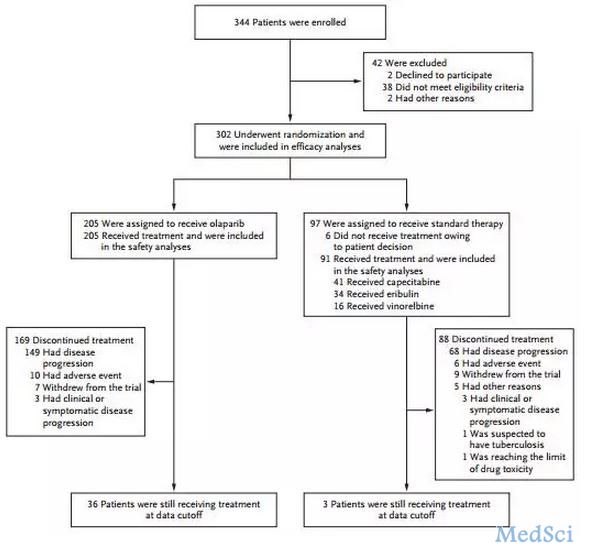
近期相关报道提示,致病性胚系BRCA1/2突变的携带者,罹患一类罕见子宫内膜癌(浆液性)的风险增高。近日《JNCI》杂志发表了一项来自法国的前瞻性队列研究,在进行了预防性输卵管和卵巢切除术后的BRCA1/2携带者中,评估子宫内膜癌的发病风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#携带者#
31
#预防性#
29
#内膜#
22
#NCI#
29
#卵巢切除术#
35
#风险降低#
0
#输卵管#
27
#切除术#
26
学习了谢谢!!
66
#BRCA突变#
28