盘点:近期有关急性冠脉综合征指南及研究一览
2016-10-10 MedSci MedSci原创
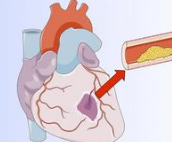
急性冠状动脉综合征(ACS)是一种常见的严重的心血管疾病,是冠心病的一种严重类型。常见于老年、男性及绝经后女性、吸烟、高血压、糖尿病、高脂血症、腹型肥胖及有早发冠心病家族史的患者。ACS患者常常表现为发作性胸痛、胸闷等症状,可导致心律失常、心力衰竭、甚至猝死,严重影响患者的生活质量和寿命。如及时采取恰当的治疗方式,则可大大降低病死率,并减少并发症,改善患者的预后。本文梅斯医学小编为大家盘点相关
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













很好。
56
好文章,分享了
57
分享了,谢谢
44
#综合征#
29
正在学习
51
好文章,受益
37
很好,谢谢,很有帮助。
31
很好,谢谢,很有帮助。
21
谢谢分享,急性非ST段抬高急性冠脉综合征患者光学相干断层扫描引导PCI比血管造影引导的PCI有较高的术后血流储备分数
31
学习啦,
22