World J Gastrointest Oncol:胃癌分子学、遗传学和免疫特征研究进展
2018-09-05 月下荷花 肿瘤资讯
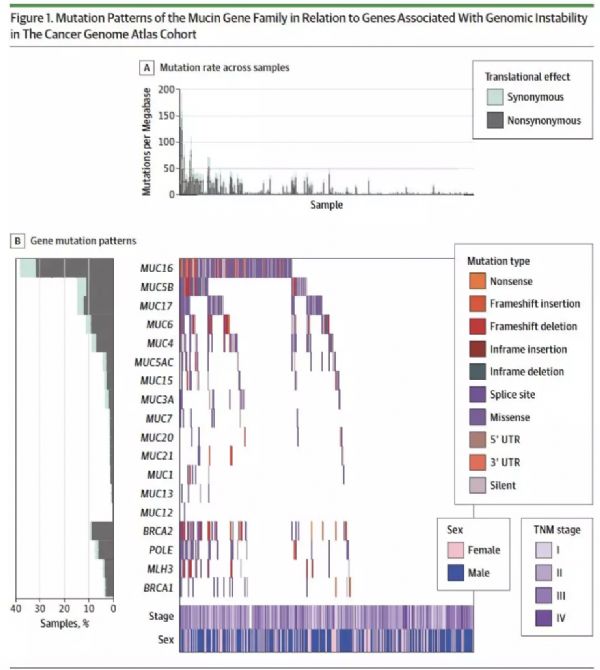
虽然近年胃癌(GC)治疗有很多进步,但多数转移性疾病预后仍很差,因此需要更多基础研究,更好的指导分子靶向治疗和免疫治疗。2014年根据TCGA将GC分为4种分子亚型,然而其转化为临床应用的征途中,结果并不如预期辉煌,2015年根据ACRG同样将GC分为4种亚型,研究显示各亚型与临床结果相关。塞浦路斯Gkolfinopoulos教授在WJGO杂志发文对二种分类进行比较,并对相关临床研究、分子靶向治疗
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
45
#Test#
35
#AST#
26
#遗传学#
31
#EST#
0
#GAS#
26
#免疫特征#
36
#研究进展#
38
学习了谢谢
74
学学了分享一下
1