朱遂强教授:中国脑出血诊治指南2019解读:NCN 2019
2019-09-22 Violet MedSci原创
9月20日,在中华医学会第二十二次全国神经病学学术会议上,来自华中科技大学同济医学院附属同济医院的朱遂强教授对“上周刚定稿”的中国脑出血诊治指南进行了解读,其中涉及到众多临床医生关注的脑出血疾病的热点问题。血肿扩大血肿扩大(HE)定义为24h复查血肿体积较基线扩大33%或12. 5ml。HE多数在脑出血(ICH)急性期(6h内)发生;HE是ICH患者预后不佳的独立危险因素,现在与HE有关公认的
9月20日,在中华医学会第二十二次全国神经病学学术会议上,来自华中科技大学同济医学院附属同济医院的朱遂强教授对“上周刚定稿”的中国脑出血诊治指南进行了解读,其中涉及到众多临床医生关注的脑出血疾病的热点问题。
血肿扩大
血肿扩大(HE)定义为24h复查血肿体积较基线扩大33%或12. 5ml。HE多数在脑出血(ICH)急性期(6h内)发生;HE是ICH患者预后不佳的独立危险因素,现在与HE有关公认的征象为“点征(Spot Sign)”。
推荐意见:
(1)脑出血后数小时内常出现HE,加重神经功能损伤,应密切监测(I级推荐,A级证据)。
(2)CTA和增强CT的“点征”有助于预测血肿扩大风险,必要时可行有关评估(II级推荐,B级证据)。
血压升高
2013年,一项前瞻性队列研究(117例患者,平均血肿容积25ml)显示:发病6 h内收缩压≥180mmHg与血肿扩大和神经功能恶化相关。
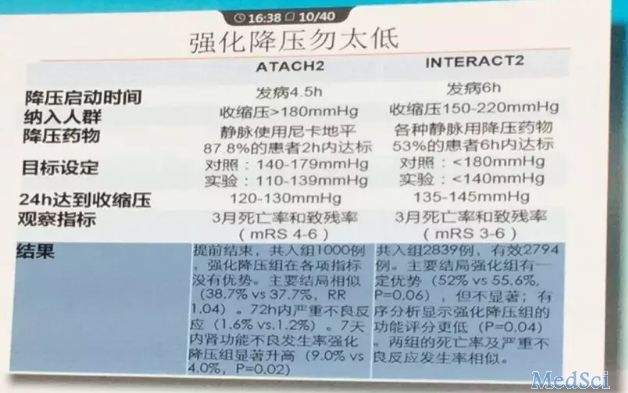
INTERACT2试验中证明急性脑出血患者早期(6h)强化降压是安全的,且能改善患者的功能结局,但强化降压不阻止HE;该试验后续分析发现平稳降压130-139mmHg获益最明显。
通过该试验与ATACH2试验对比可知,强化降压不要太低。
推荐意见:
(1)应综合管理脑出血患者的血压,分析血压升高的原因,再根据血压情况决定是否进行降压治疗( I级推荐, C级证据) ;
(2)对于收缩压150-220 mmHg的住院患者,在没有急性降压禁忌证的情况下,数小时内降压至130-140 mmHg是安全的( I级推荐, A级证据) ,其改善患者神经功能的有效性尚待进一步验证 ( II级推荐, B级证据) ;对于收缩压>220mmHg的ICH患者,在密切监测血压的情况下,持续静脉输注药物控制血压可能是合理的,收缩压目标值为160mmHg (II级推荐,D级证据)。
(3)降压治疗期间应严密观察血压水平的变化,每隔5-15分钟进行一次血压监测 (I级推荐,C级证据)。
手术治疗
STICH研究表明:与保守治疗相比,早期外科手术治疗幕上自发性ICH没有获益(OR0.89 95% CI 0.66-1.19, P=0.414) ;亚组分析显示手术对距离脑表面<1cm的脑叶血肿患者可能有益。
STICH II研究证实对于自发性浅表ICH不伴IVH的患者,早期手术并没有导致更好的临床转归(59% VS 62%; P=0.367), 仅有微弱但临床相关的生存优势。
关于小脑出血,以往研究认为对那些血肿大于3cm、伴脑干受压或脑积水的患者行手术治疗预后较好。
微创治疗
国内一项RCT研究比较了微创术联合尿激酶与开颅术治疗基底节区脑出血(30 -80 ml)的疗效,发现微创术显著降低了术后再出血风险和90天死亡率、改善患者90 d时的日常活动能力;
另一项研究对比了微创术联合尿激酶与内科保守治疗基底节区脑出血(25-40ml)的疗效,发现微创治疗明显改善了患者发病14 d时的神经功能和3个月时的功能预后。
一项纳入了15项高质量RCT试验、2152例患者的Meta分析结果显示,经过筛选的幕上 ICH 患者能够从MIS (vs.其他治疗)获益;不同技术和不同时间窗(24h内或72h内) 皆能获益。
MISTIE III试验表明手术治疗虽然不改善神经功能,但降低死亡率,残余血肿体积≦15ml可获益。
关于脑室出血的CLEAR-III试验表明EVD+rt-PA可以降低死亡率;亚组分析显示严重的IVH、清除超过80%可获益。
推荐意见:
(1)对于大多数原发性ICH患者,外科开颅手术治疗的有效性尚不能充分确定,不主张无选择地常规使用外科开颅手术(II级推荐,B级证据),微创治疗是安全的、有助于降低死亡率( I级推荐,A级证据)
(2)以下临床情况,可个体化考虑选择外科开颅手术或微创手术治疗:
1.出现神经功能恶化或脑干受压的小脑出血者,无论有无脑室梗阻致脑积水的表现,都应尽快手术清除血肿( I级推荐,B级证据) ;不推荐单纯脑室引流而不进行血肿清除(II级推荐,C级证据)
2.对于脑叶出血超过30ml且距皮质表面1cm内的患者,可考虑标准开颅术清除幕上血肿或微创手术清除血肿(II级推荐,B级证据)
3.发病72小时内、血肿体积20-40 ml、GCS≥9分的幕上高血压ICH患者,在有条件的医院,经严格选择后可应用微创手术联合或不联合溶栓药物液化引流清除血肿( II级推荐,A级证据)。
4.40 ml以上重症ICH患者由于血肿占位效应导致意识障碍恶化者,可考虑微创手术清除血肿(II级推荐,B级证据)。
5.微创治疗应尽可能清除血肿,使治疗结束时残余血肿体积≤15ml(II级推荐,B级证据)。
脑室出血
推荐意见:
EVD联合rt-PA治IVH是安全的、有助于降低重症患者的死亡率( I级推荐,A级证据),神经功能改善有待进一步研究(II级推荐,A级证据) ;联合腰穿置管引流有助于加速清除IVH、降低行脑室腹腔分流的风险(II级推荐,B级证据)。
深静脉血栓形成(DVT)
推荐意见:
(1)卧床者应注意预防DVT(I级推荐,C级证据);对疑似患者,可查D-二聚体及多普勒超声检查(I级推荐,C级证据)。
(2)鼓励患者尽早活动、腿抬高;尽可能避免下肢静脉输液,特别是瘫痪侧肢体(IV级推荐,D级证据)。
(3)入院后即应用气压泵装置,可预防深静脉血栓及相关栓塞事件(I级推荐,A级证据);不推荐弹力袜预防深静脉血栓(I级推荐,A级证据)。
(4)对易发生深静脉血栓的高危患者(排除凝血功能障碍所致的ICH患者),血肿稳定后可考虑发病后1-4天皮下注射小剂量低分子肝素或普通肝素预防深静脉血栓形成,但应注意出血的风险(II级推荐,B级证据)。
(5)当患者出现深静脉血栓或肺动脉栓塞症状时,可使用系统性抗凝治疗或下腔静脉滤器植入(II级推荐,C级证据) ;合适治疗方案的选择取决于多重因素(出血时间、血肿稳定性、出血原因及全身情况) (II级推荐, C级证据)。
抗栓和抗凝
推荐意见:
(1)需要抗栓治疗时,对合并非瓣膜性房颤的脑叶出血患者建议避免长期服用华法林抗凝治疗以防增加出血复发风险(II级推荐,B级证据)。
(2)当具有抗栓药物的明显指征时,非脑叶出血患者可以应用抗凝药物,所有ICH患者都可应用抗血小板单药治疗( II级推荐,B级证据)。
(3)当有明显的抗凝药物使用指征时,抗凝药物相关性ICH重启抗凝治疗的最佳时间尚不明确。在非机械性瓣膜患者中,至少在4周内应避免口服抗凝药物(II级推荐,B级证据)。如果有使用指征,ICH后数天可开始阿司匹林单药治疗,尽管其最佳使用时间尚不清楚(II级推荐,B级证据)。
脑出血发病急,病情变化快,致残致死率高,给患者家庭及社会带来沉重的负担,国内外研究者仍在不懈地完善脑出血诊治策略。据朱遂强教授介绍,该版指南是经过反复修订而来的,小M对比了下,该版指南与前几版指南部分细节及证据等级是有区别的,完整版请大家等待指南正式发布!
更多精彩内容,请持续关注梅斯医学!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








非常不错
39
#朱遂强#
29
#NCN#
33
#诊治指南#
31
学习了
93