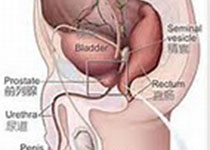
J Surg Oncol:根治性前列腺切除术后尿失禁修复术的全国性的和基于人群的研究
2017-09-12 AlexYang MedSci原创
最近,有研究人员进行了旨在评估根治性前列腺切除术(RP)后尿失禁(PPI)手术的使用情况和调查了该手术使用相关的因素。群体研究是在瑞典男性前列腺癌数据库(PCBaSe)中进行的,这些病人是在1998年和2012年年间进行初次的RP。PPI修正术过程在病人注册处进行鉴定。另外,研究人员还评估了PPI外科手术的风险比(HR)和95%的置信区间(CIs)。研究发现,26280名男性中的782名(3%)男
最近,有研究人员进行了旨在评估根治性前列腺切除术(RP)后尿失禁(PPI)手术的使用情况和调查了该手术使用相关的因素。群体研究是在瑞典男性前列腺癌数据库(PCBaSe)中进行的,这些病人是在1998年和2012年年间进行初次的RP。PPI修正术过程在病人注册处进行鉴定。另外,研究人员还评估了PPI外科手术的风险比(HR)和95%的置信区间(CIs)。研究发现,26280名男性中的782名(3%)男性患者在RP后平均3年时间后进行了PPI手术。在2000年到2014年,PPI手术的绝对值增加了8倍,并且在每1000RPs中,PPI手术增加了3倍。PPI手术的高度使用相关因素为年龄大于70岁,HR为1.96(1.54-2.50),以及高RP容量(>100 RPs每年),HR为0.81(0.66-0.99)。另外,在每1000 RPs中,最高使用地区和最低使用地区在PPI手术的使用上具有10倍的差异。在病人报道的结果测量(PROM)男性亚群中,7%的男性报道了重度PPI,并且他们中的24%经历了PPI手术。最后,研究人员指出,所有男性中的3%接受了PPI手术,卫生服务提供者之间也具有1
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#切除术#
35
#Oncol#
23
#修复术#
31
#前列腺切除#
30
#尿失禁#
27
#根治#
26
学习.谢谢分享
58