GW-ICC2017︱全面解读心律失常治疗之创新
2017-10-15 佚名 国际循环
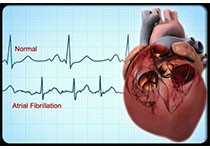
心律失常作为心血管领域的常见病及心源性猝死的主要原因之一,其多样性、复杂性及隐匿性常给临床诊治带来不小的难度。近年来,诊疗水平的不断进步使得治疗手段的选择和应用都更加合理化和个体化,日新月异的发展势头也对临床工作者提出更高要求。在本届GW-ICC 2017的美国华裔心脏协会(CNAHA)@GW-ICC联合论坛上,来自斯坦福大学的Paul J Wang教授就这一热点问题作了精彩的专场解析。下面带您一
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










学习
62
#创新#
30
#ICC#
25
#GW-ICC#
33