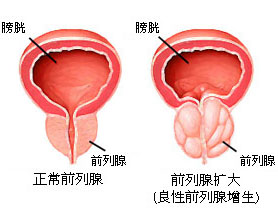
ASTRO 2016:中危前列腺癌患者接受近距离放疗就足够了
2016-09-28 Moon 译 MedSci原创
ASTRO年会上的数据显示:对于中度风险前列腺癌患者,近距离放射治疗基础上添加外照射治疗,并不能显著延长患者的无进展生存期。因此,只需要短距离放射治疗就能为这一类人群提供足够的癌症控制,并且长期不良事件更少。 德保罗医疗中心的Bradley Prestidge博士和同事们假设,中危前列腺癌患者在短距离放射治疗基础上添加外照射治疗、或组织植入放射性粒子,以周围健康组织的限制辐射暴露,与仅仅接受
ASTRO年会上的数据显示:对于中度风险前列腺癌患者,近距离放射治疗基础上添加外照射治疗,并不能显著延长患者的无进展生存期。因此,只需要短距离放射治疗就能为这一类人群提供足够的癌症控制,并且长期不良事件更少。
德保罗医疗中心的Bradley Prestidge博士和同事们假设,中危前列腺癌患者在短距离放射治疗基础上添加外照射治疗、或组织植入放射性粒子,以周围健康组织的限制辐射暴露,与仅仅接受短距离放射治疗的患者相比,5年无进展生存期(PFS)可改善10%。
研究者对579名男性(平均年龄67岁)中危前列腺癌患者的数据进行了分析,患者的临床分期为T1c (67%)到T2b,格里森评分在2-6之间+PSA在10-20之间,或格里森评分为7+PSA低于10(89%)。
患者随机分为近距离放射治疗(n = 292)或盆腔区域接受45 Gy外照射治疗(n = 287)。近距离放射治疗使用放射性碘-125或钯-103,接受外照射治疗的患者,其近距离放射治疗的剂量为110或100-Gy;仅仅接受近距离放射治疗的患者,其剂量为146-Gy或125-Gy。
PFS作为主要研究终点。中位随访期为6.7年。研究人员对443例患者长达5年的随访数据进行了分析评估。
66例患者经历了首次治疗失败,其中联合近距离放射治疗+外照射治疗组患者占34例,仅仅近距离放射治疗组患者占32例。
总体而言,联合近距离放射治疗+外照射治疗组和仅仅近距离放射治疗组患者的5年PFS率分别为85% (95% CI, 80-89)和86% (95% CI, 81-90)(HR = 1.02; P-futility = .0006)。
两组急性2级或更严重的毒性(28% vs. 27%)和急性3级或更严重的毒性(均为8%)没有组间差异。但是,联合近距离放射治疗+外照射治疗组发生迟发型2级或更严重的毒性(53% vs. 37%; P = .0001)和迟发型3级或更严重的毒性(12% vs. 7%; P = .039)的患者比例更高。联合近距离放射治疗+外照射治疗组经历3级或更糟的泌尿生殖毒性(7% vs. 3%)的患者比例更高,不过两组的3级或更严重的胃肠道毒性具有可比性(3% vs. 2%)。
原始出处:
Prestidge BR, et al. Abstract 7. Presented at: ASTRO Annual Meeting; Sept. 25-28, 2016; Boston.
Brachytherapy alone can control intermediate-risk prostate cancer.Healio.September 27, 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#AST#
36
#近距离放疗#
37
#近距离#
35
继续关注
61
继续学习
61
继续关注!
54
谢谢分享!
67