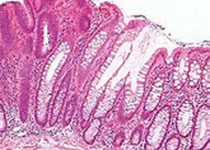
卵巢的上皮肿瘤是冰冻切片实验室中最常见的妇科标本之一。卵巢肿块的术前诊断检查通常仅限于影像学研究和血清标志物,然而两者灵敏度和特异性都比较低。因此,术中冰冻切片评估对于确定所需的手术范围至关重要,良性肿瘤的膀胱切除术,年轻患者的卵巢交界性肿瘤的卵巢切除术或有限的手术分期以保持生育力,或卵巢癌的广泛分期程序。卵巢上皮肿瘤可能表现出广泛的形态模式,它们之间往往相互重叠,并可与多种其他卵巢非上皮肿瘤类似。准确的冰冻切片诊断及结合仔细的大体检查、对形态学检查结果的适当取样和解释以及对临床背景的熟悉时术中会诊成功的关键。
本研究的目的回顾卵巢上皮肿瘤的显着冰冻切片诊断特征,特别关注有用的临床病理学和形态学线索以及潜在的诊断缺陷。
结果表明卵巢肿瘤的冷冻切片评估对实践病理学家是重大的诊断挑战。本研究详细讨论了粘液性,浆液性,子宫内膜样和卵巢透明细胞瘤的术中冰冻切片评估中最常见的临床情况和诊断问题。
原始出处:
Natalia Buza, Frozen Section Diagnosis of
Ovarian Epithelial Tumors: Diagnostic Pearls and Pitfalls
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#卵巢上皮#
27
#上皮肿瘤#
29
#Pathol#
24
#Med#
30
学习
54
学习了,谢谢作者分享!
52
学习了,谢谢分享
61