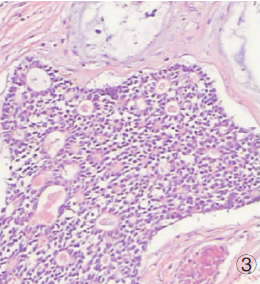
颅内类似脑膜瘤的涎腺导管癌1例
2019-01-23 刘维生 周稳 李爱军 国际神经病学神经外科学杂志
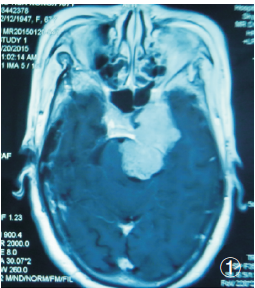
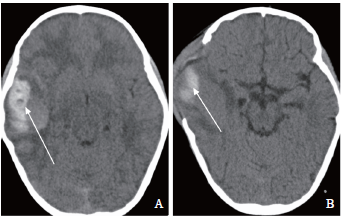
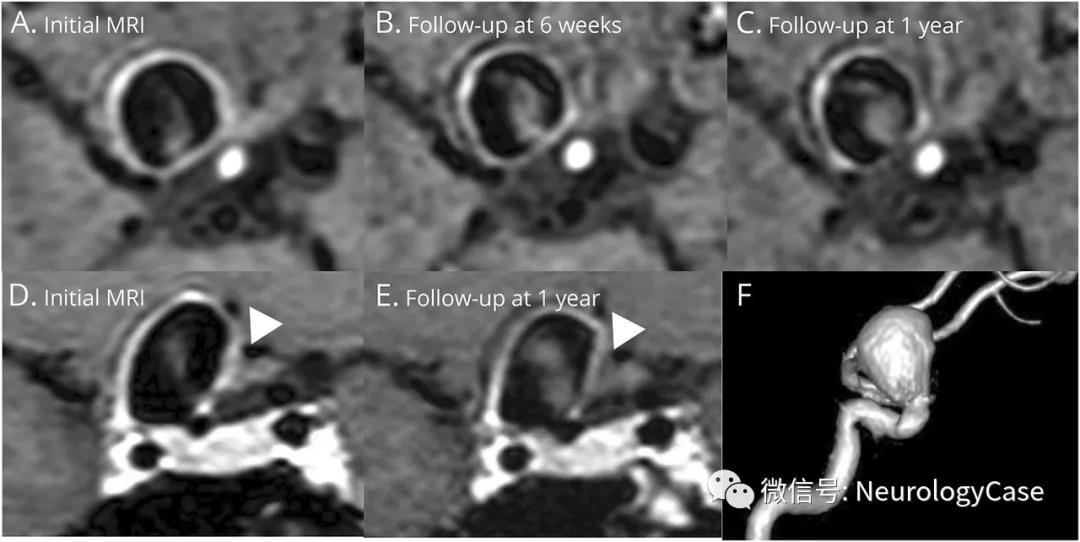
患者,女性,67岁,因“左眼睑下垂10月,头晕伴呕吐半月”入院,既往有慢支病史。查体:左动眼、滑车、展神经麻痹,右侧肢体肌力IV级。颅脑MRI:左侧岩尖区哑铃型长T1、等T2异常信号,病灶明显均匀强化(图1)。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#涎腺#
40
#脑膜瘤#
33
#涎腺导管癌#
38
好文,值得点赞!认真学习了,把经验应用于实践,为患者解除病痛。
65