PNAS:干细胞研究新进展或可加快治疗运动神经元疾病
2012-04-10 towersimper 生物谷
来自英国爱丁堡大学、伦敦大学国王学院、美国哥伦比亚大学和旧金山大学的科学家们利用前沿干细胞研究方法取得一项研究突破,从而可能会加快人们开发出治疗运动神经元疾病(motor neurone disease, MND)的新方法。 中国细胞生物学学会干细胞生物学分会2012年春季会议 他们从一名患有遗传性MND疾病的病人身上提取皮肤细胞,并利用提取到的皮肤细胞构建出运动神经元。 他们证实在90%以

来自英国爱丁堡大学、伦敦大学国王学院、美国哥伦比亚大学和旧金山大学的科学家们利用前沿干细胞研究方法取得一项研究突破,从而可能会加快人们开发出治疗运动神经元疾病(motor neurone disease, MND)的新方法。
中国细胞生物学学会干细胞生物学分会2012年春季会议
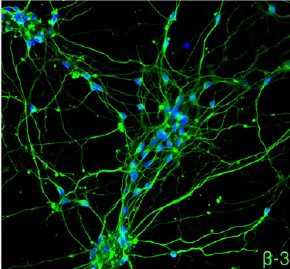
他们从一名患有遗传性MND疾病的病人身上提取皮肤细胞,并利用提取到的皮肤细胞构建出运动神经元。
他们证实在90%以上的MND病例中发现的蛋白TDP-43异常导致运动神经元死亡。这也是科学家们首次能够观察到蛋白TDP-43异常直接对人运动神经元产生影响。相关研究结果于2012年3月26日发表在PNAS期刊上。
MND疾病是一种破坏性的、不可治疗的和最终致命性的疾病,是由于控制运动、语言和呼吸的运动神经元的渐近性丢失而导致的。
爱丁堡大学教授Siddharthan Chandran说,“利用病人干细胞在盘碟中构建MND疾病模型有助于我们研究这种可怕疾病的病因以及加快药物开发。” (生物谷:towersimper编译)

doi:10.1073/pnas.1202922109
PMC:
PMID:
Mutant induced pluripotent stem cell lines recapitulate aspects of TDP-43 proteinopathies and reveal cell-specific vulnerability
Bilada Bilican, Andrea Serio, Sami J. Barmada, Agnes Lumi Nishimura, Gareth J. Sullivan, Monica Carrasco, Hemali P. Phatnani, Clare A. Puddifoot, David Story, Judy Fletcher, In-Hyun Park, Brad A. Friedman, George Q. Daley, David J. A. Wyllie, Giles E. Hardingham, Ian Wilmut, Steven Finkbeiner, Tom Maniatis, Christopher E. Shaw, and Siddharthan Chandran
Transactive response DNA-binding (TDP-43) protein is the dominant disease protein in amyotrophic lateral sclerosis (ALS) and a subgroup of frontotemporal lobar degeneration (FTLD-TDP). Identification of mutations in the gene encoding TDP-43 (TARDBP) in familial ALS confirms a mechanistic link between misaccumulation of TDP-43 and neurodegeneration and provides an opportunity to study TDP-43 proteinopathies in human neurons generated from patient fibroblasts by using induced pluripotent stem cells (iPSCs). Here, we report the generation of iPSCs that carry the TDP-43 M337V mutation and their differentiation into neurons and functional motor neurons. Mutant neurons had elevated levels of soluble and detergent-resistant TDP-43 protein, decreased survival in longitudinal studies, and increased vulnerability to antagonism of the PI3K pathway. We conclude that expression of physiological levels of TDP-43 in human neurons is sufficient to reveal a mutation-specific cell-autonomous phenotype and strongly supports this approach for the study of disease mechanisms and for drug screening.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











谢谢分享
11
#运动神经元疾病#
38
#PNAS#
38
#运动神经元#
30