Int J Rheum Dis:超声检查结果与炎症性肌病具有相关性
2017-08-12 佚名 Medicalxpress
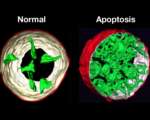
根据8月7日在国际风湿性疾病杂志上发表的一项研究,超声检查结果似乎与特发性炎症性肌病(IIM)的疾病活动具有良好的相关性,可能是患者评估的有用工具。
原始出处:
Sousa Neves J, Santos Faria D, Cerqueira M, et al.Relevance of ultrasonography in assessing disease activity in patients with idiopathic inflammatory myopathies.Int J Rheum Dis. 2017 Aug 7. doi: 10.1111/1756-185X.13150. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#相关性#
31
#检查结果#
33
#Dis#
22
讲解的非常好,值得学习
52
学习一下谢谢分享
52
#超声检查#
24
#炎症性#
21
#肌病#
30
学习了谢谢分享
43
学习一下
37