Cell丨清华王宏伟组揭示人源Dicer蛋白的工作机制——王艳丽、麻锦彪点评
2018-04-27 BioArt BioArt
这又是一个“十年磨一剑”的故事。对RNA干扰过程略有了解的读者一定不会对识别并切割pre-miRNA底物生成成熟siRNA的Dicer蛋白陌生。然而此前,Dicer蛋白的全长蛋白一直没有高分辨率结构。2009年,王宏伟教授当时还在UC伯克利做博后的时候,曾首次获得过低分辨率的Dicer-TRBP-Ago复合物 的"L" 型结构,一晃将近10年过去了,王宏伟在清华的实验室经过不断的努力和反复实验终于
这又是一个“十年磨一剑”的故事。对RNA干扰过程略有了解的读者一定不会对识别并切割pre-miRNA底物生成成熟siRNA的Dicer蛋白陌生。然而此前,Dicer蛋白的全长蛋白一直没有高分辨率结构。2009年,王宏伟教授当时还在UC伯克利做博后的时候,曾首次获得过低分辨率的Dicer-TRBP-Ago复合物 的"L" 型结构,一晃将近10年过去了,王宏伟在清华的实验室经过不断的努力和反复实验终于通过单颗粒重构技术获得了apo-hDicer-TRBP复合体的高分辨率三维结构 (4.4 ?),首次解析了人源Dicer的高分辨率整体结构,确定了Dicer蛋白中各结构域的精确三维分布及结构域之间的空间关系。 该研究称得上Dicer领域的一项里程碑式的重要进展,为了让读者更好的了解该工作的重要意义,BioArt特别邀请到了两位长期从事RNA相关结构生物学研究的专家进行点评,以飨读者!
小RNA分子介导的基因沉默(RNA-induced gene silencing)是由短片段RNA分子与 Argonaute蛋白家族,以及其他蛋白形成RISC(RNA-induced gene silencing complex)复合体;通过碱基互补配对的原则,RISC复合体在小RNA分子引导下识别、结合相应的靶RNA,并进一步通过Argonaute蛋白降解RNA或者抑制RNA翻译,从而导致靶基因低表达 (Carthew and Sontheimer, 2009; Filipowicz, 2005)。2006年,Andrew Fire和Craig Mello因为他们对RNA干扰现象的发现获得了诺贝尔医学与生理学奖。如今,小RNA介导的基因沉默技术已经成为基因功能研究的利器,并在医药、农业、畜牧业等领域广泛应用。
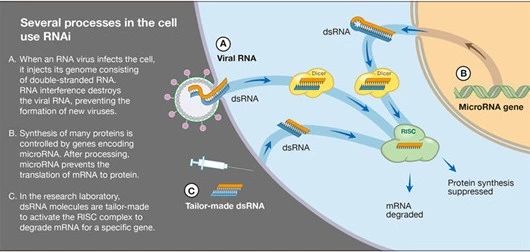
人源细胞中与Argonaute蛋白相结合的成熟小RNA 的双链具有典型的共同特征:长度约为22nt。根据小RNA的来源,可以分为内源性和外源性的小RNA。外源性的小RNA来源于长双链RNA,长双链RNA进入细胞内被Dicer蛋白识别并切割生成成熟的siRNA; 内源性的小RNA则主要是miRNA。miRNA可以有多条生成途径,其中经典的miRNA生成途径是miRNA基因在细胞核内转录生成pri-miRNA,在细胞核内被Drosha-DGCR8复合体加工生成pre-miRNA;pre-miRNA在转运蛋白作用下从细胞核进入细胞质,被Dicer蛋白识别切割生成成熟的miRNA (Carthew and Sontheimer, 2009; He and Hannon, 2004)。
到目前为止,人体内已经发现多达1800种miRNA,在个体的生长、发育、代谢等几乎所有生理过程中发挥重要的基因表达调控作用 (Friedman et al., 2009; Griffiths-Jones, 2006)。这些miRNA的前体分子在序列,二级结构,以及三级结构上都不相同,然而经过人体内唯一的一种Dicer蛋白的加工后生成为具有共同特征的双链小RNA。不同的pre-miRNA底物如何被人源Dicer精确加工的机制至今仍然不清晰,解析人源Dicer蛋白的三维结构对于了解人源Dicer蛋白的工作机制具有重要的作用。
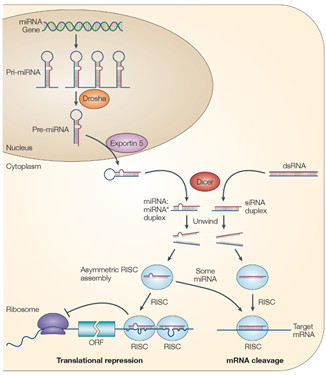
The biogenesis and post-transcriptional suppression of microRNAs and small interfering RNAs (He and Hannon, 2004)
4月26日,Cell 杂志以研究长文(Research Article)的形式发表了清华大学生命学院、北京结构生物学高精尖创新中心王宏伟研究组题为 Cryo-EM structure of human Dicer and its complexes with a pre-miRNA substrate(《人源Dicer与Dicer-pre-miRNA复合体的冷冻电镜结构》 )的研究论文,文章中首次报道了人源Dicer蛋白的全长高分辨率结构。
在这项工作发表之前,Dicer蛋白的全长蛋白一直没有高分辨率结构。过去10年的时间里,王宏伟实验室以及其他课题组都尝试运用单颗粒电镜的方法去解析人源Dicer的三维结构,并获得了该蛋白低分辨率的三维结构,呈L字型,只能大致判断结构域的三维空间分布位置 (Lau et al., 2012; Liu et al., 2015; Taylor et al., 2013; Wang et al., 2009)。该蛋白质一直没有获得高分辨率三维结构的主要原因有以下几点:
① 人源Dicer蛋白约为220kDa,对于运用单颗粒重构的方法来获的高分辨率三维结构来说,分子量还是相对比较小;
② Dicer蛋白三维结构呈L型,没有对称性,蛋白颗粒在冰中分布多为长条型,衬度低,不容易取得均一分布的冷冻样品;
③ 而且蛋白分子在冷冻样品中具有严重的优势取向,对单颗粒三维重构形成了很大的技术障碍。
王宏伟实验室经过近10年的摸索,解决了蛋白质分离纯化、冷冻样品制备、冷冻电镜数据收集以及单颗粒结构解析等多方面的技术难题,最终采用从哺乳动物293F细胞系中共表达人源Dicer和TRBP蛋白复合体,应用Strep亲和层析分离纯化蛋白质,使用纯金载网或者镀金载网制备hDicer-TRBP复合体的冷冻样品等手段,制备出了分布较为均一、优势取向相对较少的冷冻电镜样品。王宏伟实验室成员利用单颗粒重构技术获得了apo-hDicer-TRBP复合体的高分辨率三维结构 (4.4 ?)(图1),首次解析了人源Dicer的高分辨率整体结构,确定了Dicer蛋白中各结构域的精确三维分布及结构域之间的空间关系。
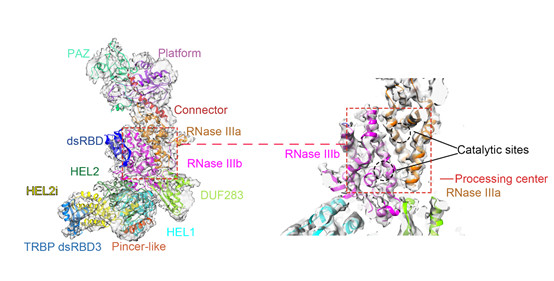 图1. Human Dicer-TRBP complex
图1. Human Dicer-TRBP complex为了更进一步了解人源Dicer蛋白是如何加工pre-miRNA底物的过程,通过体外重组、制备冷冻样本、单颗粒重组等技术,王宏伟教授课题组进一步获得了hDicer-TRBP-pre-let-7复合体的三维结构,发现hDicer-TRBP-pre-let-7复合体中pre-let-7存在两种明显不同的结构状态:一种是pre-let-7的茎部呈完全互补结构(hDicer-TRBP-pre-let-7 complex class I),另一种是pre-let-7的茎部呈部分解离的状态(hDicer-TRBP-pre-let-7 complex class II)(图2)。
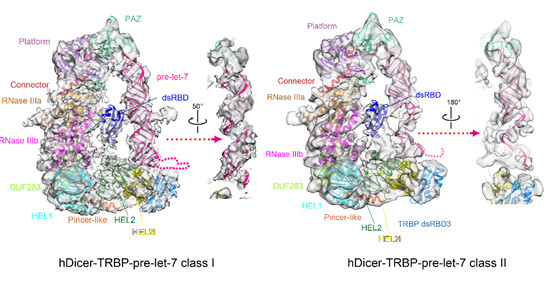
图2. Human Dicer-TRBP-pre-let-7 complexes
王宏伟课题组与清华大学张强锋实验室合作,通过icSHAPE、RNase酶切、测序胶电泳等实验,发现pre-let-7在溶液中呈动态的构象平衡,一部分pre-let-7的茎部是完全互补的双链螺旋结构, 也有一部分pre-let-7的茎部是呈部分解离的状态。深入的研究表明hDicer-TRBP复合体与pre-let-7结合可以促进RNA向茎部完全互补的状态转换,确保RNA茎部结构的一致性,从而保证加工RNA的精确性。
进一步的,王宏伟课题组还发现hDicer的DExD/H-box helicase 结构域有Helicase 1、Helicase 2i以及Helicase 2构成,呈C字型。通过氨基酸序列比对分析,DEXD/H-box helicase 结构域与RIG-I、MDA5在氨基酸序列上具有高度保守些,三维结构同样具有高度相似性。因此,他们提出DExD/H-box helicase结构域作用于RNA底物的方式与RIG-I、MDA5等蛋白具有相似性的假说。生化实验证实hDicer的DEXD/H-box helicase 结构域对蛋白的酶切活性具有重要的影响。
专家点评
王艳丽(中科院生物物理所PI,国家杰青,HHMI国际学者)
Comments:自从上世纪90 年代RNA干扰发现以来,广大科学家对RNA干扰通路进行了非常系统的研究,但是由于高等生物的Dicer 蛋白的复杂性,导致Dicer 蛋白如何加工前体小RNA形成成熟小RNA一直是个悬而未决的问题。宏伟的这篇工作非常的及时和漂亮,回答了大家等待已久的小RNA 加工这一核心问题!早在2009年,宏伟首次报道了低分辩率的Dicer-TRBP-Ago复合物 的"L" 型结构,近10年后的今天, 宏伟的研究团度进一步解析了Dicer-TRBP-pre-Let7复合物原子分辨率的结构,首次揭示了Dicer-TRBP 复合物促进前体小RNA 的稳定,发现了Dicer蛋白的解螺旋酶结构域的调控功能。这一研究结果是RNA干扰领域的又一个重大突破,填补了RNA干扰作用机理的一大空白,促进人们对RNA干扰机理的进一步理解。
Comments:Dicer蛋白作为多种非编码小RNA(miRNA,siRNA及部分tsRNA)产生过程中最重要的酶,长久以来缺少和底物的复合物的高分辨三维结构。清华大学王宏伟实验室最新发表在Cell杂志的人Dicer蛋白及其与miRNA前体(pre-miRNA)复合物的高分辨率冷冻电镜结构,首次清晰呈现了Dicer与底物结合的近似活性状态。依赖于冷冻电镜的优势,两种不同的pre-miRNA底物的构象被捕捉到,非常有意思的是,其中一种构象与最近发表在Science上的果蝇Dicer2与底物的复合物冷冻电镜结构类似,在HEL2结构域附近发生了RNA双螺旋的解旋。另一种pre-miRNA的构象保持了颈环结构的双螺旋部分,但由于3'末端结合PAZ结构域的取向使其偏离了Dicer的RNaseIII活性中心大约30度。为了能够获得直观的Dicer剪切底物的构象,通过结合人Dicer的PAZ模块与双链RNA的晶体结构(Mol Cell,2011)和AaRNaseIII与双链RNA底物的复合物晶体结构,模拟了人Dicer剪切双链RNA底物的结构模型,清楚地说明了人Dicer剪切产物是~20bp长度。总之,王宏伟实验室的高分辨冷冻电镜结构是Dicer研究的里程碑式的成果,为进一步理解Dicer的作用机制提供了基础。
原始出处:
Zhongmin Liu, Jia Wang, Hang Cheng, et al.Cryo-EM Structure of Human Dicer and Its Complexes with a Pre-miRNA Substrate.cell.2018.4.26
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#DIC#
38
#Cell#
34
#工作机制#
45
#ICER#
40
#CEL#
0
学习一下谢谢分享
55
#清华#
0
学习了新知识
53
学习了新知识
56
学习了新知识
64