Nat Mater:哈佛大学新型癌症疫苗促进有效DC细胞识别与免疫记忆形成
2018-05-31 佚名 生物极客
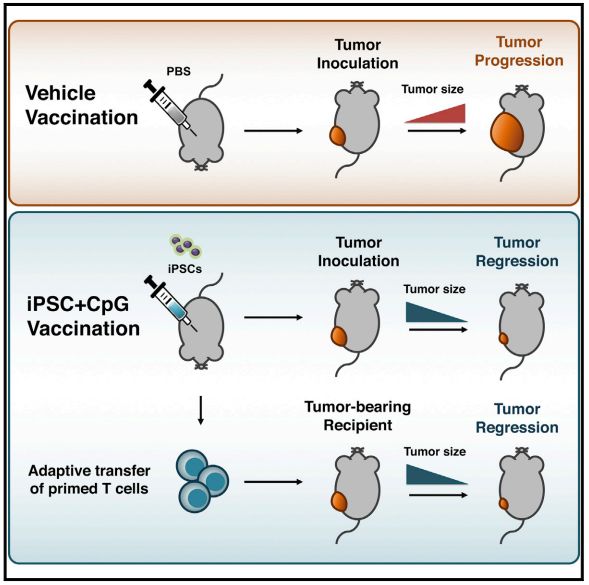
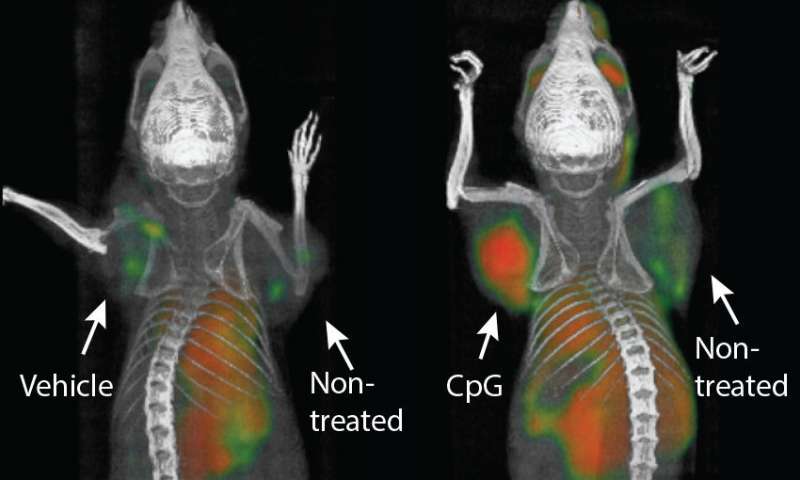
免疫疗法正在走向癌症治疗的前沿。根据哈佛大学的一项新研究,最近的临床试验已经证明,这些方法可以针对每个人的肿瘤的独特突变情况进行个性化治疗,从而为许多患者点燃新的希望。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Nat#
27
#DC细胞#
50
#哈佛#
33
学习了谢谢
73
学习了受益匪浅
75
^_^^_^^_^
67