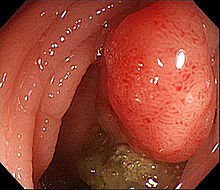
SCI REP:术中芬太尼用量不会影响结直肠癌患者预后
2017-09-08 MedSci MedSci原创
阿片类药物是治疗肿瘤相关疼痛及围手术期急性疼痛的主要止痛药。但是有研究表明阿片类药物会抑制人体细胞及体液免疫功能。尽管目前尚无直接证据证明阿片类在肿瘤发生中的作用,但是动物模型中已发现其可能会导致肿瘤复发。芬太尼也有同样的促肿瘤特性。SCI REP近期发表了一篇文章,研究术中芬太尼用量对结直肠癌患者预后的影响。
阿片类药物是治疗肿瘤相关疼痛及围手术期急性疼痛的主要止痛药。但是有研究表明阿片类药物会抑制人体细胞及体液免疫功能。尽管目前尚无直接证据证明阿片类在肿瘤发生中的作用,但是动物模型中已发现其可能会导致肿瘤复发。芬太尼也有同样的促肿瘤特性。SCI REP近期发表了一篇文章,研究术中芬太尼用量对结直肠癌患者预后的影响。研究共回顾性分析了2011年1月到2014年12月之间共1679例Ⅰ-Ⅲ期接受肿瘤切除的结直肠癌患者。利用风险回归模型分析术后无复发生存和总生存情况。研究结果表明芬太尼用量与无复发生存和总生存之间无剂量依赖联系。通过平均芬太尼用量将患者分为高剂量组和低剂量组,两组间无复发生存和总生存无显着区别。文章最后认为,术中芬太尼用量对结直肠癌患者肿瘤切除后无复发生存或总生存无影响。原始出处:Ying-Hsuan Tai,Hsiang-Ling Wu,et al.Intraoperative Fentanyl Consumption Does Not Impact Cancer Recurrence or Overall Survival after Curative Colorectal
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#患者预后#
38
学习了.谢谢分享
65
#芬太尼#
41
#结直肠#
44
谢谢分享.学习了
79