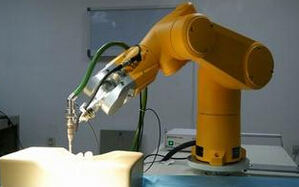
Lancet:机器人辅助腹腔镜前列腺切除术vs开放性耻骨后前列腺根治切除术
2016-07-27 MedSci MedSci原创
缺乏机器人辅助腹腔镜前列腺切除术和开放耻骨后前列腺根治切除术的实验数据比较是泌尿肿瘤学领域的重要知识缺口。我们旨在比较这两种方法的功能预后和肿瘤结局及术后12周时的早期结局。
缺乏机器人辅助腹腔镜前列腺切除术和开放耻骨后前列腺根治切除术的实验数据比较是泌尿肿瘤学领域的重要知识缺口。我们旨在比较这两种方法的功能预后和肿瘤结局及术后12周时的早期结局。
此3期随机对照试验,入组标准为,皇家布里斯本与妇女医院(Brisbane, QLD)新近诊断为局限前列腺癌,选择手术作为治疗方式,能够阅读和说英语,无头部受伤史、痴呆史、或精神疾病史或其他合并的癌症,估计生存期超过10年或更久,年龄35-70岁的男性。受试者随机分配为接受机器人辅助腹腔镜前列腺切除术或开放耻骨后前列腺根治切除术。这是开放手术,研究的数据分析人员对每个患者的情况是不知情的。除此之外,病理学家对接收到的活检或开放切除样本是不知情的。主要终点是6周、12周和24个月时泌尿道功能(泌尿道调查表EPIC)和性功能(性功能EPIC和IIEF调查表),以及肿瘤预后(阳性手术边缘状态和24个月时疾病进展的生化和影像学证据)。这个实验是为了评估超过24个月的健康相关和泌尿系统特异性生活质量。现在报告的是6周和12周的早期结局。
在2010年8月23日到2014年11月25日,163人随机分配到开放耻骨后前列腺根治切除术,163人接受机器人辅助腹腔镜前列腺切除术。18人退出(两组分别为12人和6人);因此,151人参加了开放手术组,157人参加机器人辅助组。开放手术中121完成了12周的调查问卷vs机器人辅助手术组131人。两组间泌尿功能评分无显著差异,6周时分别为, (74·50 vs 71·10; p=0·09),12周时 (83·80 vs 82·50; p=0·48)。两组间性功能评分无显著差异,分别为,6周时 (30·70 vs 32·70; p=0·45),12周时(35·00 vs 38·90; p=0·18)。两组间等效检测差异分别为,15 [10%] vs 23 [15%],基于90% CI, Δ为10%,表明两种手术是不等效的。开放手术组14人 (9%)vs机器人辅助组6人 (4%)有术后并发症 (p=0·052)。开放手术组12 (8%) 人vs机器人辅助组3 (2%)人发生术中不良事件。
结论:两组手术12周时的近期功能预后相近。仍需观察长期随访结果,我们让患者和亲属自行选择信任的手术方式,而不推荐某一种手术。
原始出处:
John W Yaxley, FRACS, Geoffrey D Coughlin,et al,Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: early outcomes from a randomised controlled phase 3 study,Published Online: 26 July 2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#前列腺切除#
38
#切除术#
31
文章不错
67
科研与临床结合
61
#Lancet#
28
继续关注
56
厉害的研究
0
#腹腔镜#
26
#机器人#
25
#机器人辅助#
26