ATS/ERS/JRS/ALAT四学会共发发布:特发性肺纤维化治疗指南更新
2015-10-17 MedSci MedSci原创
表2015年与2011年IPF治疗指南推荐变化情况 美国胸科学会(ATS)/欧洲呼吸学会(ERS)/日本呼吸学会(JRS)/拉丁美洲胸科学会(ALAT)于近日联合对2011年特发性肺纤维化(IPF)治疗临床实践指南进行了更新,文章发表于《美国呼吸与重症医学杂志》(AJRCCM)。 2015年9月27日欧洲呼吸学会(ERS)年会上,该指南修订委员会主席华盛顿大学医学中心加内什?拉古(Gane
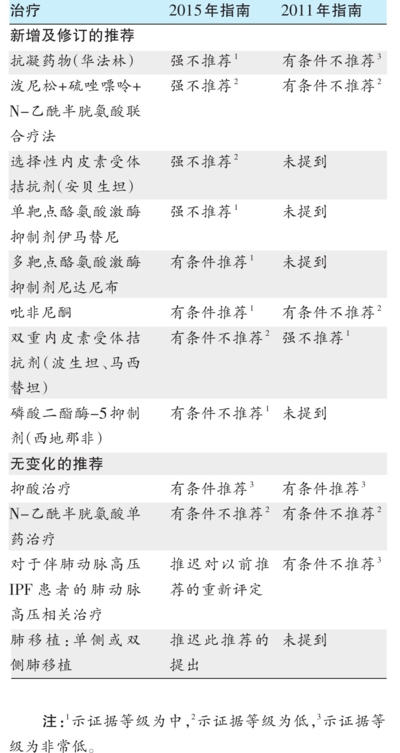
表2015年与2011年IPF治疗指南推荐变化情况
美国胸科学会(ATS)/欧洲呼吸学会(ERS)/日本呼吸学会(JRS)/拉丁美洲胸科学会(ALAT)于近日联合对2011年特发性肺纤维化(IPF)治疗临床实践指南进行了更新,文章发表于《美国呼吸与重症医学杂志》(AJRCCM)。
2015年9月27日欧洲呼吸学会(ERS)年会上,该指南修订委员会主席华盛顿大学医学中心加内什?拉古(Ganesh Raghu)教授对指南的部分推荐意见及更新要点进行了介绍,受到与会者的极大关注。
指南的部分推荐意见及更新要点问答
问题1:IPF患者是否应该接受抗凝药物治疗?
推荐意见:除非患者有其他已知的需要抗凝治疗的适应证,否则不推荐IPF患者使用华法林进行抗凝治疗(强烈建议反对,低级别证据)。
理由和实施注意事项:增加的死亡风险要求强烈建议反对使用口服华法林治疗IPF。该建议仅适用于目标为国际标准比值(INR)2.0~3.0的口服华法林治疗,不包括针对其他适应证的其他抗凝药物。患者若有需要使用抗凝药物的其他已知适应证,例如静脉血栓栓塞性疾病或心房颤动,则应遵循相应指南治疗。
问题2:IPF患者是否应接受酪氨酸激酶抑制剂伊马替尼治疗?
推荐意见:不推荐IPF患者使用伊马替尼进行治疗(强烈建议,中等级别证据)。
理由和实施注意事项:药物价格相对昂贵,且尚无证据表明该药能够使IPF患者在预防疾病进展或死亡方面获益。
问题3:IPF患者是否应该接受泼尼松、硫唑嘌呤和N-乙酰半胱氨酸联合治疗?
推荐意见:不推荐临床医生在IPF患者中使用泼尼松、硫唑嘌呤和N-乙酰半胱氨酸联合治疗(强烈建议,低级别证据)。
理由和实施注意事项:该建议主要基于一项因不良反应而提前终止的单一研究。虽然研究被提前终止,仅招募了50%入选患者,但还是清楚地显示了对患者多项重要转归有负面影响。
问题4:IPF患者是否应该接受选择性内皮素受体拮抗剂安贝生坦治疗?
推荐意见:不管患者是否存在肺动脉高压,均不推荐在IPF患者中使用安贝生坦进行治疗(强烈建议反对,低级别证据)。
理由和实施注意事项:由于安贝生坦的适应证为肺动脉高压,而非IPF。指南制定委员会不推荐将安贝生坦用于有肺动脉高压临床表现的IPF患者。鉴于缺乏获益证据且有潜在危害,建议正在使用安贝生坦治疗的IPF患者终止治疗。
问题5:IPF患者是否应接受酪氨酸激酶抑制剂尼达尼布治疗?
推荐意见:建议在IPF患者中使用尼达尼布进行治疗(有条件推荐,中等级别证据)。
理由和实施注意事项:主要基于尼达尼布对患者重要预后指标有改善作用,例如采用用力肺活量(FVC)下降率评估的疾病进展程度以及死亡率,不着重考虑药物潜在的不良反应和治疗费用。
用药前应告知患者尼达尼布的不良反应,例如腹泻。目前证据主要集中在肺功能(PFT)为轻-中度受损的患者中,且治疗长期影响尚属未知。
问题6:IPF患者是否应该接受吡非尼酮治疗?
推荐意见:建议使用吡非尼酮对IPF患者进行治疗(有条件推荐,中等级别证据)。
理由和实施注意事项:该意见重点强调了吡啡尼酮对患者重要预后指标的改善,例如采用FVC下降率评估患者的疾病进展程度和死亡率,不着重考虑药物的严重不良反应和治疗费用。
吡啡尼酮的不良反应较广,即便是FVC评估治疗受益的情况下,部分患者仍不能忍受某种不良反应,因此开始治疗前,应就不良反应进行患者教育。此外,目前吡啡尼酮治疗费用较高,在做出治疗决定时,特别是患者直接承担治疗的经济负担时,必须将这一影响因素考虑进去。
问题7:IPF患者是否应该接磷酸二酯酶-5抑制剂西地那非治疗?
推荐意见:不建议在IPF患者中使用西地那非治疗(有条件不推荐,中等级别证据)。
理由和实施注意事项:尽管西地那非对患者生活质量有轻微改善,但其对死亡率、急性加重、呼吸困难无改善,且其相关不良反应和治疗费用也是潜在的障碍。
问题8:IPF患者是否应接受内皮素受体A和B双重拮抗剂波生坦或马西替坦治疗?
推荐意见:不建议在IPF患者中应用内皮素受体A和B双重拮抗剂波生坦或马西替坦(有条件不推荐,低级别证据)。
理由和实施注意事项:该建议强调了该药对患者重要预后指标的改善情况和高昂的治疗费用,对其降低患者死亡风险和延缓疾病进展考虑较少。鉴于患者各项预后指标改善的不一致性(死亡率和疾病进展),以及效果评估欠准确,委员会不推荐该治疗。
原始出处:
Spagnolo P, Bonella F, Maher TM.New guideline on treatment of idiopathic pulmonary fibrosis. Lancet Respir Med. 2015 Sep;3(9):e31-2.
Raghu G, Rochwerg B, Zhang Y, Garcia CA, Azuma A, Behr J, Brozek JL, Collard HR, Cunningham W, Homma S, Johkoh T, Martinez FJ, Myers J, Protzko SL, Richeldi L, Rind D, Selman M, Theodore A, Wells AU, Hoogsteden H, Schünemann HJ; ATS, ERS, JRS, and ALAT.An Official ATS/ERS/JRS/ALAT Clinical Practice Guideline: Treatment of Idiopathic Pulmonary Fibrosis. An Update of the 2011 Clinical Practice Guideline. Am J Respir Crit Care Med. 2015 Jul 15;192(2):e3-19.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








学习了,很好
101
#特发性#
42
#ALA#
36
#治疗指南#
35
#ATS#
0
#指南更新#
36
#ERS#
39
为了积分我也是拼了~
183
赞一个~
137
这篇文章写得很好
116