Nature Commun:协助引起各种癌症的“帮凶”——TET2
2017-04-25 Heather_z727 medicalxpress
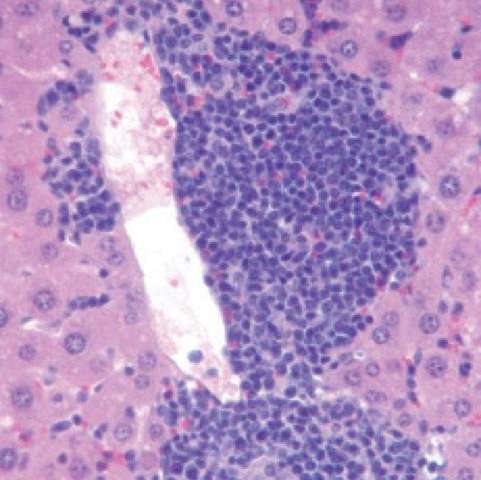
【科学家找到了刺激癌症形成的催化剂】想象一下这个场景:在高速公路上,司机突然想转向,然后意识到自己的错误,迅速转向,已经来不及了。其他司机们都来不及反应,因此开始发生碰撞。这一场景就好像各种血癌中TET2蛋白质的情况,TET2可以抑制肿瘤,阻止造血干细胞疯涨,然而,如果TET2发生突变,它还会引起其他基因突变,TET2的突变并不会直接致癌,但是却为癌症的形成创造了条件。研究人员表示:“如果你只是失
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#TET#
35
#COMMUN#
38
#Nat#
26
#TET2#
36
继续学习新机制
69