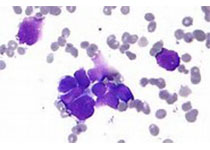
Blood:研究人员发现可鉴别多发性骨髓瘤患者对哪种治疗方案更敏感的基因印迹
2018-09-05 MedSci MedSci原创
中心点:研究人员推断出一种7基因印迹,可鉴别对硼替佐米或以来那度胺为基础的疗法更敏感的骨髓瘤患者。根据印迹治疗的效果不次于采用硼替佐米、来那度胺和地塞米松联合治疗。摘要:改善多发性骨髓瘤患者的预后不仅要开发新的疗法,更要更好的应用现有的治疗措施。Michael A. Chapman等人采用II期PADIMAC(以硼替佐米、阿霉素和地塞米松[PAD]联合治疗未进行过治疗的多发性骨髓瘤患者:延期ASC
中心点:
研究人员推断出一种7基因印迹,可鉴别对硼替佐米或以来那度胺为基础的疗法更敏感的骨髓瘤患者。
根据印迹治疗的效果不次于采用硼替佐米、来那度胺和地塞米松联合治疗。
摘要:
改善多发性骨髓瘤患者的预后不仅要开发新的疗法,更要更好的应用现有的治疗措施。Michael A. Chapman等人采用II期PADIMAC(以硼替佐米、阿霉素和地塞米松[PAD]联合治疗未进行过治疗的多发性骨髓瘤患者:延期ASCT患者的微小残留病灶[MRD]的影响)研究招募的新确诊的患者的样本,进行RNA测序(RNA-Seq)。
研究人员利用合成退火和大边界最近邻算法,开发了一种7基因印迹来预测治疗预后,并在采用以硼替佐米和来那度胺为基础的疗法治疗的独立队列中验证该印迹。
该印迹可区分哪些患者对哪种疗法的反应性更好。在CoMMpass(将多发性骨髓瘤临床预后与个人遗传图评估联系起来)数据集中,与传统治疗的患者相比,根据印迹正确治疗的患者的无进展存活期和总体存活期均更长(中位值:20.1个月 vs 未达到,危险比 0.40,95% CI 0.23-0.72,p=0.0012;30.7个月 vs 未达到,危险比 0.41,95% CI 0.21-0.80,p=0.0049)。
总而言之,上述根据印迹正确治疗的患者的预后并不次于采用硼替佐米、来那度胺和地塞米松联合(美国的标准疗法)治疗的患者。该印迹仅包含7个基因,便于应用于临床,有助于指导更多的靶向药物应用于骨髓瘤。
原始出处:
Michael A. Chapman,et al. RNA-Seq of newly diagnosed patients in the PADIMAC study leads to a bortezomib/lenalidomide decision signature. Blood 2018 :blood-2018-05-849893; doi: https://doi.org/10.1182/blood-2018-05-849893
本文系梅斯医学(MedSci)原创编译,转载需授权!
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#多发性#
25
#治疗方案#
39
#研究人员#
29
嗯嗯,学习了。
61