Mol Cell:揭示明星分子RB在肿瘤中的新功能
2018-12-07 生物君 iNature
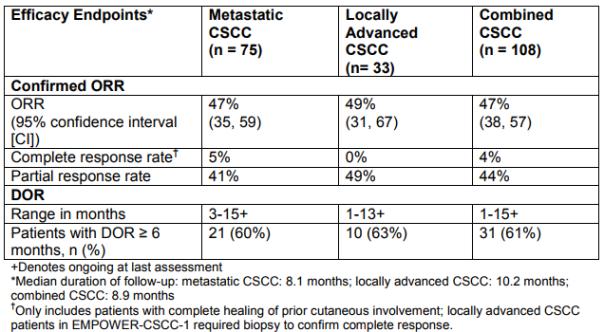
程序性死亡配体-1(PD-L1)在肿瘤细胞中的异常表达通过抑制癌症免疫来促进癌症进展。视网膜母细胞瘤蛋白RB是已知调节细胞周期,DNA损伤反应和分化的肿瘤抑制因子。2018年12月7日,华中科技大学Wu Heshui,江苏大学附属医院Zhu Runzhi及美国梅奥诊所黄浩杰共同通讯在Mol Cell在线发表题为“Phosphorylated RB Promotes Cancer Immunity
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Cell#
34
#新功能#
43
#CEL#
39
认真学习,不断进步,把经验分享给同好。点赞了!
98