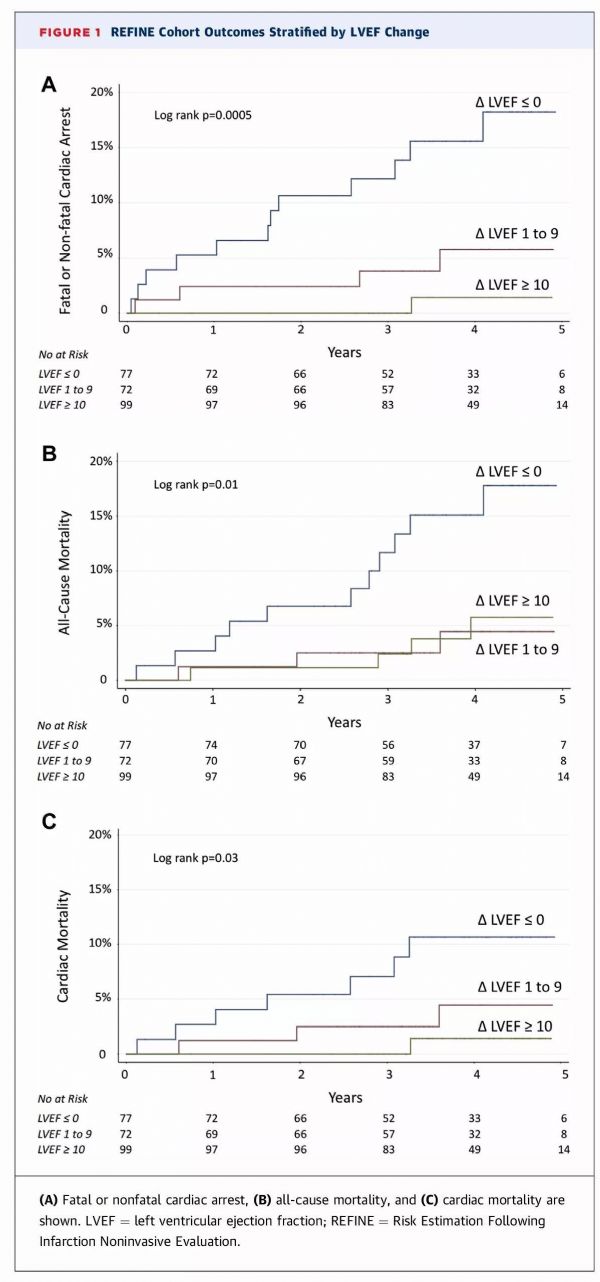
JACC:首发心肌梗死后左心室射血分数改变可影响患者预后
2018-03-08 国际循环编辑部 国际循环
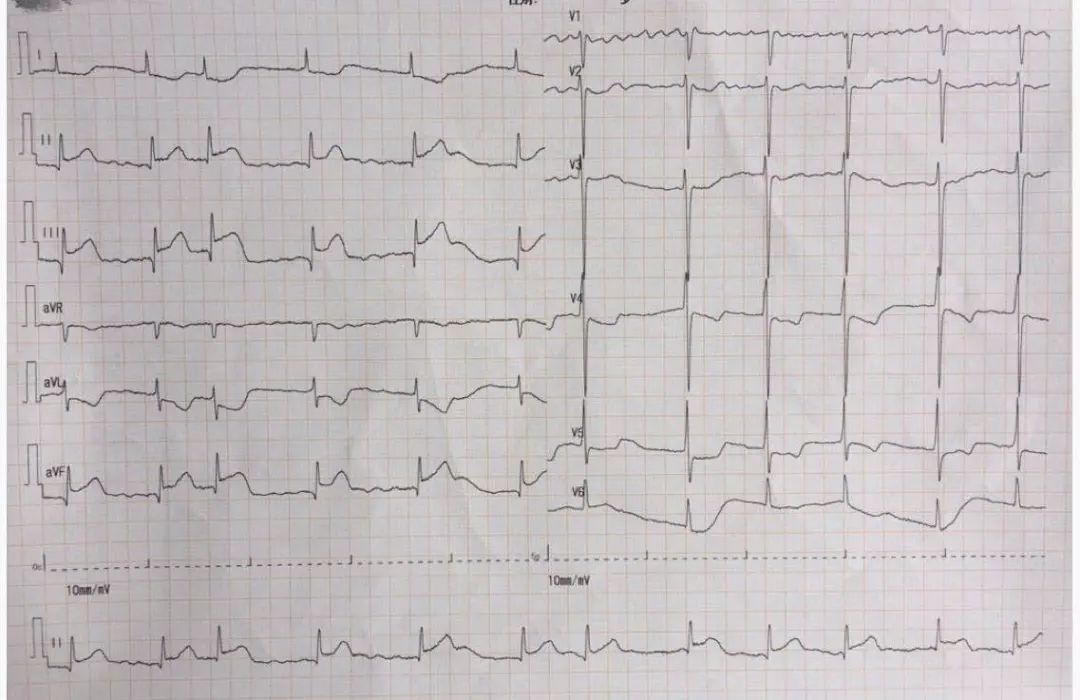
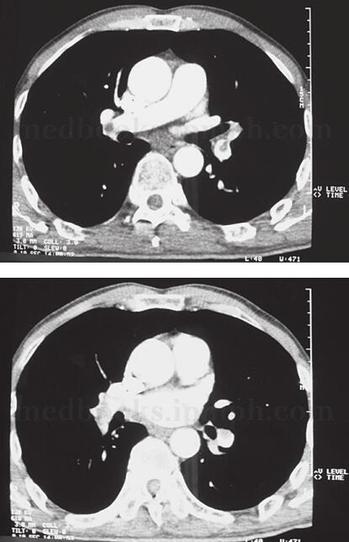
心肌梗死(MI)后早期左心室射血分数(LVEF)降低有助于识别存在不良结局风险的患者,但MI后数周到数月LVEF变化能否为患者预后提供额外信息尚不清楚。近期,JACC发表的一项最新研究探讨了首发MI后LVEF变化对患者预后的影响。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#患者预后#
29
#JACC#
20
#左心室射血分数#
37
#ACC#
26
#左心室#
30
学习了.谢谢
56
学习了很有用不错
47