Cell Metab:TXNIP分子为糖尿病治疗提供新的靶点
2012-08-14 T.Shen 生物谷
从最基本的层面上来说,糖尿病是一种具有压力特征的疾病,这种压力是细微的压力,可以引发患者产生炎症以及使患者胰腺分泌的胰岛素水平降低。 如今来自加利福尼亚大学的研究者发现了一种方法糖尿病这种压力的新的关键分子-硫氧还蛋白互作蛋白(TXNIP),其在糖尿病早期可以方法这种压力效应,而且对于炎症反应非常重要,可以引发机体产生胰岛素的胰腺细胞死亡。这种分子不光可以产生压力、放大压力而且可以使得结果更坏,

从最基本的层面上来说,糖尿病是一种具有压力特征的疾病,这种压力是细微的压力,可以引发患者产生炎症以及使患者胰腺分泌的胰岛素水平降低。
如今来自加利福尼亚大学的研究者发现了一种方法糖尿病这种压力的新的关键分子-硫氧还蛋白互作蛋白(TXNIP),其在糖尿病早期可以方法这种压力效应,而且对于炎症反应非常重要,可以引发机体产生胰岛素的胰腺细胞死亡。这种分子不光可以产生压力、放大压力而且可以使得结果更坏,研究者的相关研究刊登在了近日的国际杂志Cell Metabolism上。

新分子TXNIP的发现为以后开发新型的药物提供了新的靶点,研究者也认为这种新药靶点计划惠及很多糖尿病早期患者,当糖尿病开始发现或者已经开始发展的时候,这个时间段成为“蜜月时期”。
临床试验已经揭示了饮食或者其它途径的改变可以延长某些患者的糖尿病“蜜月期”以及阻止某些人糖尿病的发生,研究者的目的是发现一种方法来延长这种“蜜月期”。
糖尿病以及β细胞的缺失
糖尿病是美国人群的一个主要的健康问题,在美国影响着8.3%人群的健康,每年治疗这种疾病会花掉纳税人2000亿美元。仅在加州就有400万人患II型糖尿病,而且数百万人都有患糖尿病的风险。这些数字足矣使得研究者开发出新的疗法或者药物来治疗糖尿病或者预防糖尿病。
糖尿病的核心就是特殊的激素产生细胞-β细胞,其位于机体胰腺中,可以产生胰岛素来帮助调节机体血糖水平。β细胞就像小的生物工厂一样可以大量产生胰岛素。一个单独的β细胞就可以每分钟产生100万个胰岛素分子。
如果β细胞缺失了,胰腺就不会产生足够的胰岛素来维持机体的血糖水平,长期如此就会导致糖尿病的发生。
编译自:A molecule central to diabetes is uncovered

doi:10.1016/j.cmet.2012.07.007
PMC:
PMID:
IRE1α Induces Thioredoxin-Interacting Protein to Activate the NLRP3 Inflammasome and Promote Programmed Cell Death under Irremediable ER Stress
Alana G. Lerner, John-Paul Upton, P.V.K. Praveen, Rajarshi Ghosh, Yoshimi Nakagawa, Aeid Igbaria, Sarah Shen, Vinh Nguyen, Bradley J. Backes, Myriam Heiman, Nathaniel Heintz, Paul Greengard, Simon Hui, Qizhi Tang, Ala Trusina, Scott A. Oakes, Feroz R. Papa
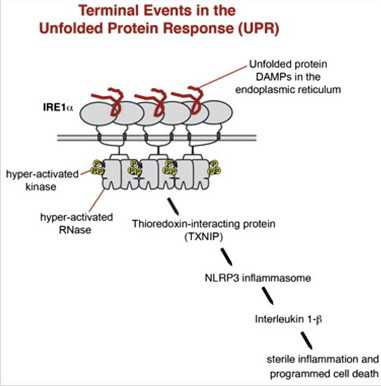
When unfolded proteins accumulate to irremediably high levels within the endoplasmic reticulum (ER), intracellular signaling pathways called the unfolded protein response (UPR) become hyperactivated to cause programmed cell death. We discovered that thioredoxin-interacting protein (TXNIP) is a critical node in this terminal UPR. TXNIP becomes rapidly induced by IRE1α, an ER bifunctional kinase/endoribonuclease (RNase). Hyperactivated IRE1α increases TXNIP mRNA stability by reducing levels of a TXNIP destabilizing microRNA, miR-17. In turn, elevated TXNIP protein activates the NLRP3 inflammasome, causing procaspase-1 cleavage and interleukin 1β (IL-1β) secretion. Txnip gene deletion reduces pancreatic β cell death during ER stress and suppresses diabetes caused by proinsulin misfolding in the Akita mouse. Finally, small molecule IRE1α RNase inhibitors suppress TXNIP production to block IL-1β secretion. In summary, the IRE1α-TXNIP pathway is used in the terminal UPR to promote sterile inflammation and programmed cell death and may be targeted to develop effective treatments for cell degenerative diseases.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#Meta#
39
#糖尿病治疗#
29
#Cell#
37
#CEL#
28
#MET#
39