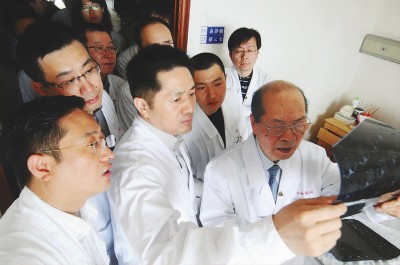
中科院院士樊嘉:门诊不限号 手术敢闯“禁区”
2017-11-29 李雪林、陈青 文汇报
中国科学院2017年新增院士昨天揭晓,新增院士樊嘉在肝肿瘤领域树起标杆。樊嘉有哪些创新感悟呢?
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#中科院#
28
学习了
60
这是有多少僵尸
50
非常好的文章.学习了
55
学习榜样
53
好资料学习了!
62
学习了.谢谢
15