Circ-Heart Fail:心衰患者服用Sacubitril/缬沙坦的情况分析!
2018-02-20 xing.T MedSci原创
由此可见,sacubitril /缬沙坦经食品药品监督管理局批准后使用率较低,可能与高成本相关。
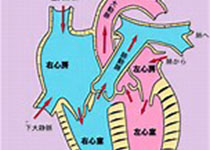
2015年7月,美国食品和药物管理局批准Sacubitril(脑啡肽酶抑制剂)/缬沙坦用于射血分数降低的心力衰竭患者。近日,心血管领域权威杂志Circ-Heart Fail上发表了一篇研究文章,研究人员的目的是评估Sacubitril /缬沙坦自通过食品和药物管理局批准后的最初18个月内使用和处方药费用情况。
研究人员采用美国大型保险数据库确定了2015年7月1日和2016年12月31日之间以sacubitril /缬沙坦为第一个处方的患者。研究人员将其与接受血管紧张素转换酶抑制剂或血管紧张素受体阻滞剂治疗的患者进行比较。结果包括使用、处方药成本以及180天的依从性,定义为服用比例≥80%。
该研究共有2244例患者开始服用sacubitril/缬沙坦。虽然用户数随时间的增加而增加,但是射血分数降低的心力衰竭患者服用sacubitril/缬沙坦治疗比例仍较低(<3%)。开出sacubitril/缬沙坦处方的患者较为年轻,更常见为男性,比那些服用血管紧张素转换酶抑制剂或血管紧张素受体拮抗剂的合并症更少。虽然处方费用大部分由医疗计划支付(每30天处方费用的平均数为328.37美元;中位数为 362.44美元),但自费费用仍然很高(平均数为71.16美元;中位数为40.27美元)。通过比较,赖诺普利、氯沙坦、卡维地洛和螺内酯平均自付费用为2美元至3美元。总体而言,59.1%的患者坚持服用sacubitril/缬沙坦。填充模式显示近一半的依从性差的患者在开始服用sacubitril/缬沙坦治疗180天内停药。
由此可见,sacubitril /缬沙坦经食品药品监督管理局批准后使用率较低,可能与高成本相关。
原始出处:
Lindsey R. Sangaralingham,et al. Adoption of Sacubitril/Valsartan for the Management of Patients With Heart Failure. Circulation:heart failure. 2018. https://doi.org/10.1161/CIRCHEARTFAILURE.117.004302
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#sacubitril/缬沙坦#
34
#Sacubitril#
46
#ART#
37
#缬沙坦#
42
#心衰患者#
39
#HEART#
26
学习
39
好好好学习学习
39
成本太高.老百姓用不起
36
学习
47