Blood:brentuximab vedotin治疗复发或难治性系统性间变性大细胞淋巴瘤的2期临床报告
2017-10-07 MedSci MedSci原创
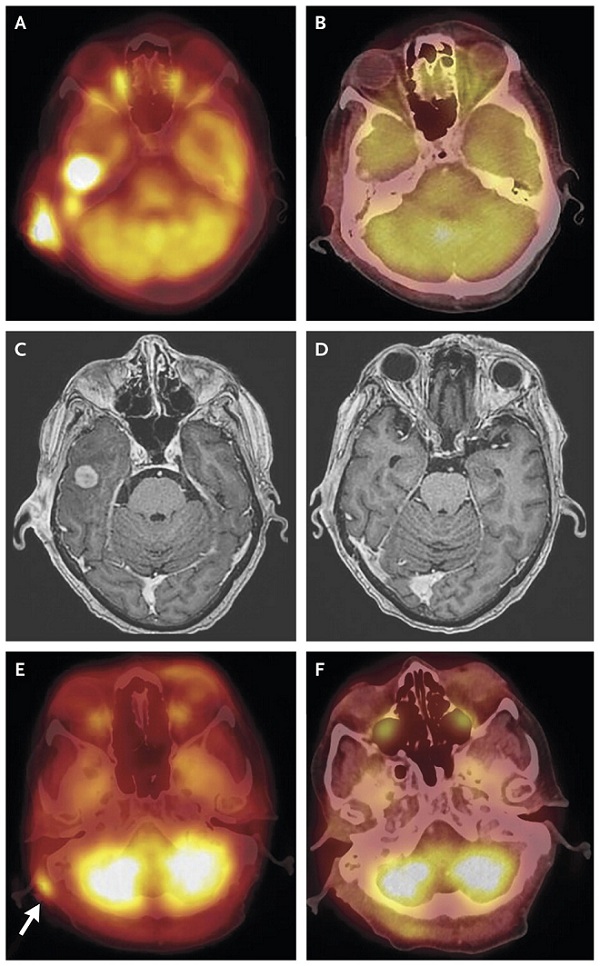
brentuximab vedotin 是新型靶向抗体 - 药物偶联物,能使药物直接作用于淋巴瘤细胞上的靶点 CD30,美国食品和药品监督管理局 2011 年 8 月 19 日批准其上市。这个关键的2期研究,评估了治疗复发或难治性系统性间变性大细胞淋巴瘤(ALCL)患者时,brentuximab vedotin的安全性和疗效。在第一次治疗后约为6年的中位观察期里,研究人员监测了患者的缓解期、无进展
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#mAb#
31
#2期临床#
19
#细胞淋巴瘤#
30
#系统性#
27
#Brentuximab#
38
#变性#
32
#vedotin#
26
#难治性#
29