每日病例丨一例骨科罕见疾病
2017-11-06 MedSci MedSci原创
这是一种罕见的病因不明的慢性进行性骨病变,以骨小梁被纤维组织逐渐取代为特点的自限性良性骨疾病,好发于儿童和青年,女性多见。病史:患者为一位24岁的年轻女性,5年前无明显诱因及原因出现右侧胸背部钝痛,上肢活动牵拉时加重,无咳嗽、咳痰及痰中带血。无午后低热,无畏寒、发热,无盗汗、乏力,无头晕、头痛,无恶心、呕吐,无腹痛、腹胀等不适。当时未予重视,自服中草药治疗,效果欠佳。近年来病情渐加重,于1周前就诊
这是一种罕见的病因不明的慢性进行性骨病变,以骨小梁被纤维组织逐渐取代为特点
的自限性良性骨疾病,好发于儿童和青年,女性多见。
病史:
患者为一位24岁的年轻女性,5年前无明显诱因及原因出现右侧胸背部钝痛,上肢活动牵拉时加重,无咳嗽、咳痰及痰中带血。
无午后低热,无畏寒、发热,无盗汗、乏力,无头晕、头痛,无恶心、呕吐,无腹痛、腹胀等不适。当时未予重视,自服中草药治疗,效果欠佳。
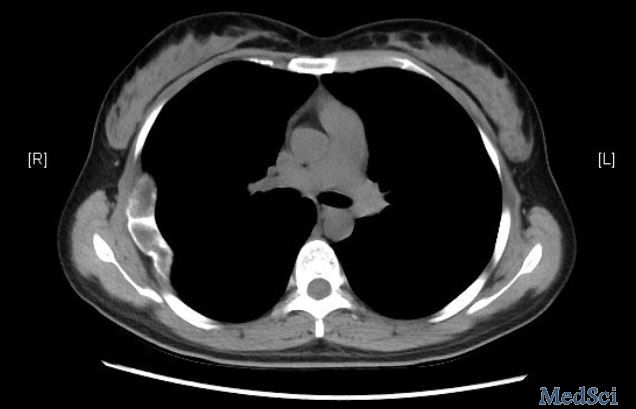
近年来病情渐加重,于1周前就诊于当地医院,行胸部CT示:右侧第5肋骨局限性膨胀,髓内密度增高;后转入我院。
查体:
发育正常,正常面容,自动体位,神志清楚,正常步态。言语清晰,精神状态安静,查体合作。双肺叩诊呈清音,听诊及双肺呼吸音清,未闻及干湿性啰音及胸膜摩擦音。心前区无隆起及凹陷,心界无扩大,心率80次/分,节律规整,各瓣膜听诊区无闻及病理性杂音。气管居中,胸廓对称无畸形,双侧胸廓呼吸动度相等,触诊语颤相等,双侧锁骨上淋巴结未触及明显肿大。脊柱无畸形,四肢无畸形,双下肢无水肿。双下肢足背动脉搏动正常。
辅助检查:
胸片:右侧第5肋骨局限性膨胀,髓内密度增高
胸部CT+重建:双肺未见异常密度,气管及主支气管通畅,纵隔肺门未经肿大淋巴结,胸腔未见积液。所见右侧第5肋骨整体不规整,走形迂曲,骨质成不规则膨胀性改变。膨胀区密度不均匀,骨皮质变薄,骨皮质尚完整,周围软组织未见异常。

血常规:白细胞计数8.23 10^9/L、血红蛋白148.0 g/L、血小板计数207 10^9/L。
大生化:谷丙转氨酶19.70 U/L、谷草转氨酶23.60 U/L、尿素7.80 mmol/L、肌酐78.00 umol/L。
简要解析:颅面骨、骨盆、长骨、肋骨为该病好发部位,其次为腓骨、肱骨、桡骨
和尺骨等,可累及单一骨骼或多处骨骼,部分多骨型可伴有内分泌症状,可引起骨软化、畸形及发生病理骨折。此病临床表现为缓慢进行性、呈膨胀性的局部骨性肿块,侵蚀骨皮质,肿块可压迫邻近器官、组织,从而出现局部骨区畸形、肿胀、疼痛等不同临床表现。
那么看到这儿,这个疾病的情况您心里有数了吗?完整病例请查看梅斯医生——骨科病例库:右侧胸背部钝痛5年余,
更多点评分析,趣味的学习,详情尽在梅斯医生上,您可以在这里体验模拟诊疗。

本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















学习了.感谢分享.
77
谢谢分享学习了
80
#罕见#
48
学习了受益匪浅!
70