Crit Care Med:心源性休克合并急性冠脉综合早期评估的新型标志物!
2017-04-15 MedSci MedSci原创
心源性休克合并急性冠脉综合征的死亡率很高,合理使用机械循环支持等先进疗法需要进行客观的风险分层。一些临床变量已被用于判断心源性休克的风险。近期,一项发表在杂志Crit Care Med上的研究旨在评估可溶性ST2和氨基末端前B型利钠肽的连续监测对心源性休克风险分层临床参数的附加意义。CardShock(www.clinicaltrials.gov NCT01374867)是一项心源性休克的前瞻性欧
心源性休克合并急性冠脉综合征的死亡率很高,合理使用机械循环支持等先进疗法需要进行客观的风险分层。一些临床变量已被用于判断心源性休克的风险。
近期,一项发表在杂志Crit Care Med上的研究旨在评估可溶性ST2和氨基末端前B型利钠肽的连续监测对心源性休克风险分层临床参数的附加意义。
CardShock(www.clinicaltrials.gov NCT01374867)是一项心源性休克的前瞻性欧洲跨国研究。主要研究了CardShock风险评分,其是由基线时的7个临床变量计算,并与短期死亡率相关。
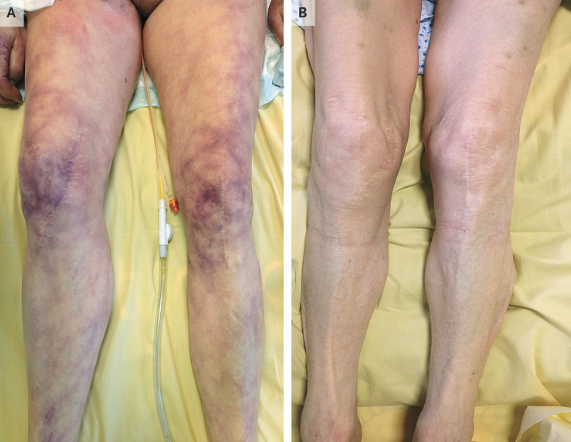
此项研究的受试对象为急性冠状动脉综合征引起的心源性休克患者(n = 145)。在此项子研究中,在ICU或心脏护理医院停留期间的八个时间点分析来自受试患者的血浆样品,评估生物标志物的额外预后价值。
此项研究显示:可溶性ST2和氨基末端前B型利尿钠肽的组合很好的区别了30天死亡率(曲线下面积为在心源性休克起始后12小时为0.77,5-10天为0.93)。12小时时,与一个或两个生物标志物均不升高相比(分别为31%或10%),两组生物标志物均升高(可溶性ST2≥500ng/ mL,氨基末端前B型利尿钠肽≥4,500ng/ L)的患者30天死亡率高(79%; p <0.001)。在12小时的时候,将可溶性ST2和氨基末端前B型利尿钠肽联合测定,加入CardShock风险评分可以重新正确分类11%的患者。
此项研究结果表明:可溶性ST2和氨基末端前B型利尿钠肽的组合提供了急性冠状动脉综合征相关心源性休克患者的临床变量之外的早期风险评估,可能有助于这些患者的治疗决策。
原始出处:
Tolppanen H, Rivas-Lasarte M, et al. Combined Measurement of Soluble ST2 and Amino-Terminal Pro-B-Type Natriuretic Peptide Provides Early Assessment of Severity in Cardiogenic Shock Complicating Acute Coronary Syndrome. Crit Care Med. 2017 Apr 11. doi: 10.1097/CCM.0000000000002336.
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#标志物#
35
#心源性休克#
0
#心源性#
32
#Med#
37