Heart:CABG中采用双边或单侧乳内动脉移植一年内成本哪个高?
2017-04-28 xing.T MedSci原创
在随机化分组之后12个月期间,采用BIMA的CABG手术患者的平均成本比采用SIMA的CABG手术患者约高出9%,主要是由于在手术室停留时间和住院时间较长,在随访期间胸骨伤口问题相关的成本并略微有所增加。对试验主要终点随访10年将揭示移植物通畅或总生存期是否存在长期差异。
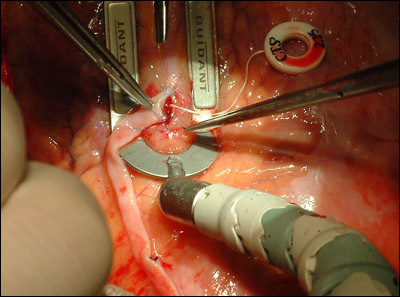
采用双侧乳内动脉(BIMA)的冠状动脉旁路移植术(CABG)可以提高患者生存率,相比于使用单侧乳内动脉冠状动脉搭桥术(SIMA)的患者,但是可能外科手术更复杂(因此更昂贵),并且与受损的胸骨伤口愈合相关。近日,在心脏病领域权威杂志Heart上发表了一篇研究文章,作为动脉血运重建(ART)试验的一部分,研究人员首次对患者12个月期间医疗资源的使用和成本进行了详细地比较。
研究人员将七个国家28家医院的3102例患者进行随机化分组,分别接受采用BIMA的CABG手术(n=1548)或采用SIMA的CABG手术(n=1554)。研究人员对详细的资源使用数据进行了收集,并覆盖了手术、最初的医院等信息,时间直至随机分组后12个月。研究人员计算了总成本,并且在试验队列和亚组间进行了比较。
随机接受采用BIMA的CABG手术患者手术时间延长了20 min(95%可信区间为15-25,P<0.001),而且还需要处理更多的胸骨伤口问题。在采用BIMA的CABG手术患者中,每名患者12个月总成本平均(SD)为£13839(£10534),而在采用SIMA的CABG手术的患者中,每名患者12个月总成本平均(SD)为£12717(£9719)(平均成本差异为£1122,95%可信区间为£407-£1838,P=0.002)。亚组和治疗分配之间的相互作用无显著性差异。
在随机化分组之后12个月期间,采用BIMA的CABG手术患者的平均成本比采用SIMA的CABG手术患者约高出9%,主要是由于在手术室停留时间和住院时间较长,在随访期间胸骨伤口问题相关的成本并略微有所增加。对试验主要终点随访10年将揭示移植物通畅或总生存期是否存在长期差异。
原始出处:
Alastair M Gray,et al. One-year costs of bilateral or single internal mammary grafts in the Arterial Revascularisation Trial. Heart. 2017.http://dx.doi.org/10.1136/heartjnl-2016-311058
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#ART#
30
#HEART#
0
好文,值得点赞,更值得收藏!慢慢领会学习的。给点个赞!
49
学习了谢谢分享
50
学习了,谢谢作者分享!
45
你的人都有自己的
41