NEJM:未绝经乳腺癌患者的内分泌治疗
2015-02-04 Mechront 译 MedSci原创
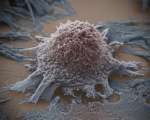
对于绝经前早期乳癌女性患者,若病灶免疫组化结果提示雌激素受体阳性或孕激素受体阳性,临床上通常会行内分泌治疗——使用药物抑制卵巢功能,减少雌激素生产,从而减少乳癌复发,但是目前对于该类患者使用添加了他莫昔芬的抑制卵巢雌激素生成疗法的疗效并不明确。因此Prudence A等人进行了一项试验,以评估对进行了完整化疗后未绝经患者以及单独使用他莫昔芬的未绝经患者,行辅助内分泌治疗是否合适。研究的初始数据分析
对于绝经前早期乳癌女性患者,若病灶免疫组化结果提示雌激素受体阳性或孕激素受体阳性,临床上通常会行内分泌治疗——使用药物抑制卵巢功能,减少雌激素生产,从而减少乳癌复发,但是目前对于该类患者使用添加了他莫昔芬的抑制卵巢雌激素生成疗法的疗效并不明确。因此Prudence A等人进行了一项试验,以评估对进行了完整化疗后未绝经患者以及单独使用他莫昔芬的未绝经患者,行辅助内分泌治疗是否合适。
研究的初始数据分析以测试研究者假设:与单独使用他莫昔芬相比,他莫昔芬加卵巢抑制可以提高无病生存率。在初始分析人群中,有46.7%的患者先前没有行化疗,53.3%的患者先前行过化疗治疗,纳入研究时仍未绝经。
该研究共纳入3066绝经前女性,根据是否化疗分为两组,随机将其分为三组,分别行以下治疗:单独使用他莫昔芬、他莫昔芬加卵巢抑制和依西美坦加卵巢抑制。平均随访67个月,5年无病生存率在他莫昔芬加卵巢抑制组为86.6%,他莫昔芬组为84.7%,两组疾病复发、继发浸润性癌或死亡危险比HR 0.83,95% CI 0.66-1.04,P=0.10。对预后影响因素进行多变量分析后,提示他莫昔芬加卵巢抑制比单独使用他莫昔芬疗效更好HR 0.78,95% CI 0.62-0.98。绝大多数复发患者先前行过化疗治疗,在这群人中,他莫昔芬加卵巢抑制组5年无病生存率为82.5%,他莫昔芬组为78.0%,复发的危险比HR 0.78,95% 0.60-1.02。依西美坦加卵巢抑制组5年无病生存率为85.7%,与他莫昔芬组相比,复发危险比HR 0.65,95% 0.49-0.87。
研究结果显示,在整体研究人群中,他莫昔芬加卵巢抑制并没有提供更好的疗效。对于仍未绝经、进行过化疗治疗、复发风险高的患者,与单独使用他莫昔芬相比,卵巢抑制加他莫昔芬将会改善疾病预后和结局。在高风险绝经前队列,与单独使用他莫昔芬相比,芳香酶抑制剂依西美坦加卵巢抑制将会降低复发风险。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#分泌#
25
不错要看看原始文章
128
不错的文章,学习了
154
已阅
128
赞
124
有意思,学习
106
#绝经#
22
#乳腺癌患者#
20
对哦,有空白对照会更好
48
如何有个空白对照组就好了
41