本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-02-12 zhangfan MedSci原创
研究证实急性胰腺炎与胰腺癌长期风险相关

美国临床内分泌医师协会(AACE)和美国内分泌学会(ACE)日前联合发表了一份共识声明,强调关于降糖药物可能增加胰腺炎和某些癌症风险的现有数据尚不足以改变临床实践。这份共识声明同时发表在《内分泌实践》杂志的在线版和纸质版上。
同时的烟草和乙醇暴露可以通过抑制未折叠蛋白信号通路导致腺泡死亡,同时激活内质网压力途径加速腺泡死亡以及胰腺炎易感
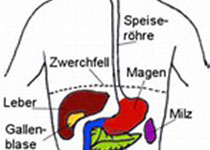
急性胰腺炎(acute pancreatitis,AP)是指多种病因引起的胰酶激活,继以胰腺局部炎性反应为主要特征,伴或不伴其他器官功能改变的疾病。临床以急性上腹痛、恶心、呕吐、发热和血清淀粉酶增高等为特点,大多数患者病程呈自限性,20%-30%患者临床经过凶险,总体病死率5%-10%。本病具有起病急、病情重、并发症多、病死率高等特点,近年来发病率有增加的趋势,是临床常见的消化系统疾病之一。目前,
研究发现对于感染性坏死性胰腺炎患者,内镜疗法在减少严重并发症或死亡方面不优于手术疗法,但内镜治疗胰瘘率降低且住院时间缩短
高淀粉酶血症是临床上经常遇到的情况,多数由急性胰腺炎所致,少数高淀粉酶血症与胰腺炎并无关联,往往因为误诊为急性胰腺炎而进行过度检查和治疗,不仅导致医疗资源不必要的浪费,而且也会对患者造成身心损伤。因此临床工作中要认真做好高淀粉酶血症病因的鉴别诊断。
胰腺炎是胰腺因胰蛋白酶的自身消化作用而引起的疾病。胰腺有水肿、充血,或出血、坏死。临床上出现腹痛、腹胀、恶心、呕吐、发热等症状。化验血和尿中淀粉酶含量升高等。这里梅斯小编整理了近期关于胰腺炎的相关研究进展,与大家一同分享。【1】乳酸林格氏液积极水合作用预防ERCP术后胰腺炎胰腺炎内镜逆行胰胆管造影(ERCP)最常见的并发症。先前评估乳酸林格氏液积极水合作用减少ERCP术后胰腺炎(PEP)发生率


梅斯医学MedSci APP
医路相伴,成就大医
#Gastroenterol#
29
#AST#
34
#GAS#
30
#长期风险#
30
#Gastroenterology#
21