BMJ Open:哪些心血管疾病治疗药物会增加老年人骨折风险?
2016-01-03 Seven L 译 MedSci原创
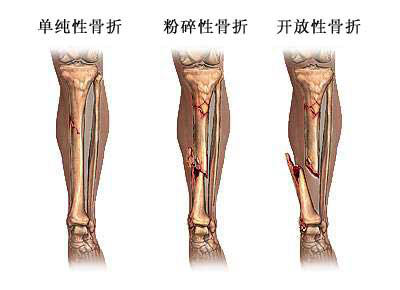
研究者进行了一项研究,探究治疗心血管疾病包括高血压等相关药物,是否会增加>65岁人群脆性骨折风险。该回顾性队列研究纳入了1 586 554名年龄>65岁的参与者。通过处方获取参与者心血管疾病相关药物(硝酸盐、地高辛、噻嗪类、呋塞米、血管紧张素转换酶抑制剂、血管紧张素受体拮抗剂、β受体阻滞剂、钙拮抗剂和他汀类药物)暴露情况,使用多因素泊松回归模型评估药物与脆性骨折风险间关系,以及校正后IRRs。研究
Torstensson M, Hansen AH,et al.Danish register-based study on the association between specific cardiovascular drugs and fragility fractures.BMJ Open. 2015 Dec 29;5(12):e009522.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#BMJ#
29
#治疗药物#
30
#PE#
37
认识了
110
#疾病治疗#
30
机制不太清楚
43
不错,赞一个
101
学会了
103
楼主给力
107
哦,
98