JBC:DES基因触发心律失常性右心室心肌病
2012-05-25 Beyond 生物谷
畸形的结蛋白与同种类的完整蛋白质相聚合从而引发骨骼肌和心肌疾病。这项研究由RUB心脏和糖尿病中心完成,领导者为Hendrik Milting博士在与同事Würzburg和 Bielefeld。他们研究报告刊登在Journal of Biological Chemistry杂志上。 一个有缺陷的基因是足以诱发疾病 通常,在细胞内结蛋白形成稳定细丝。DES基因突变后会诱发不同的肌肉疾病。由于染色体
畸形的结蛋白与同种类的完整蛋白质相聚合从而引发骨骼肌和心肌疾病。这项研究由RUB心脏和糖尿病中心完成,领导者为Hendrik Milting博士在与同事Würzburg和 Bielefeld。他们研究报告刊登在Journal of Biological Chemistry杂志上。
一个有缺陷的基因是足以诱发疾病
通常,在细胞内结蛋白形成稳定细丝。DES基因突变后会诱发不同的肌肉疾病。由于染色体总是成对出现的,每个单元的两个不同染色体上有两个DES基因。 desminopathies打破,即使只有一个DES的基因突变。运用光敏定位显微技术(PALM),研究人员阐述了其中机制。
突变和完整蛋白质可见技术
如果一个DES基因突变,而另一个未突变是完整的,细胞会同时产生畸形和正常的蛋白质。由于不仅结蛋白的突变导致蛋白质聚集在一起,但完整的结蛋白也会促进蛋白聚集,但一个有缺陷的DES基因是足以引发疾病的。使用光敏定位显微技术,研究人员将突变体和完整的蛋白质带有不同荧光分子,然后考察蛋白质变异以及完整对疾病的作用。
进一步的研究计划
下一步,研究小组想找出DES基因触发心律失常性右心室心肌病的机制。心律失常性右心室心肌病是一种罕见的心脏肌肉病,其特点是右心室严重缺陷。

doi:10.1074/jbc.M111.313841
PMC:
PMID:
Dual-color photoactivation localization microscopy of cardiomyopathy associated desmin mutants
Andreas Brodehl, Per Niklas Hedde, Mareike Dieding, Azra Fatima, Volker Walhorn, Susan Gayda, Tomo Saric, Baerbe Klauke, Jan Gummert, Dario Anselmetti, et al.
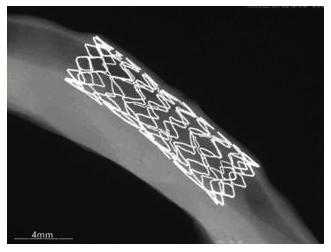
Mutations in the DES gene coding for the intermediate filament protein desmin may cause skeletal and cardiac myopathies, which are frequently characterized by cytoplasmic aggregates of desmin and associated proteins at the cellular level. By atomic force microscopy we demonstrated filament formation defects of desmin mutants, associated with arrhythmogenic right ventricular cardio-myopathy. To understand the pathogenesis of this disease, it is essential to analyze desmin filament structures under conditions in which both healthy and mutant desmin are expressed at equimolar levels mimicking an in vivo situation. Here, we applied dual-color photoactivation localization microscopy using photoactivatable fluorescent proteins genetically fused to desmin and characterized the heterozygous status in living cells lacking endogenous desmin. In addition, we applied fluorescence resonance energy transfer to unravel short-distance structural patterns of desmin mutants in filaments. For the first time, we present consistent high resolution data on the structural effects of five heterozygous desmin mutations on filament formation in vitro and in living cells. Our results may contribute to the molecular understanding of the pathological filament formation defects of heterozygous DES mutations in cardiomyopathies.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#JBC#
28
#右心室#
34
#DES#
27
#DES#
30
#肌病#
25