本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
2018-03-17 佚名 中国医学影像学杂志
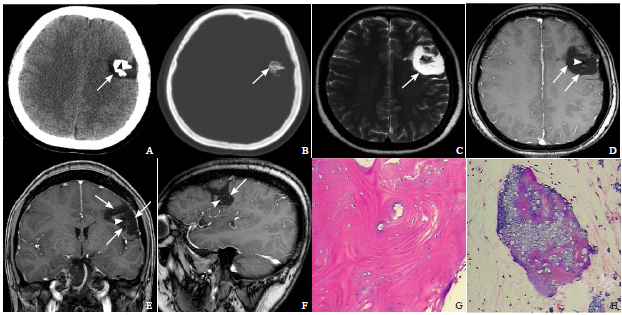
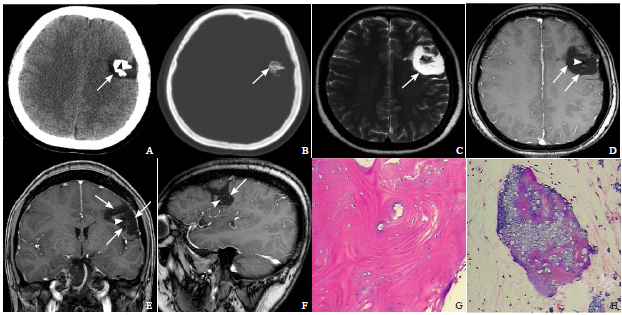
女,49岁。头部右侧受击,出现头晕、头痛,呈持续性胀痛,四肢肌力和肌张力正常。
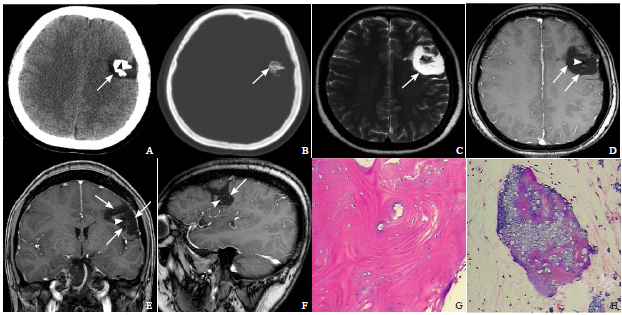

一个79岁的女人,神经功能逐渐下降1年,相关功能的下降涉及混乱、记忆力减退、不平衡和尿失禁。 查体时患者只面向自我,有轻微的迟滞型失语症。 辅助检查如下图。 计算机断层扫描(CT)显示大左额颞叶肿块伴钙化。CT血管造影和磁共振成像显示肿块(大小3.8厘米乘6.2厘米乘3.9厘米)无增强或腔内充盈,疑似血栓性动脉瘤,可能来源于大脑中动脉分叉。T2加权显示血液有分层现象。常规
男,38岁
2018年2月,发表在《Stroke》的一项由韩国和美国科学家进行的研究,考察了自发性颅内出血患者超急性期血压变异性和结局之间的相关性。
64岁,女性。动脉瘤蛛网膜下腔出血的家族史。筛查时发现左侧ICA颅内动脉瘤,随后采用血流导向装置治疗动脉瘤。
随着影像学技术的发展,数字减影血管造影(DSA)仍然作为诊断大部分脑血管病变的金标准,而CT血管造影(CTA)在诊断颅内小动脉瘤方面发挥着越来越大的作用。研究人员通过进行了该项大样本队列研究,旨在以DSA为金标准,评估CTA血管造影在诊断5mm以下的脑动脉瘤的准确性。并将研究结果发表于放射学权威杂志Radiology上。
随着ipad在患者不同身体部位上方的移动,屏幕上会随之产生出相应的图像,并最终锁定患者颅内肿瘤的具体位置,引导医生实现对肿瘤的‘精确手术’。在即将举行的2013年中国国际工业博览会上,复旦大学数字医学研究中心主任宋志坚教授及其团队展出这一最新研发成果。这一成果在国际数字医学领域尚属首创。 脑肿瘤等脑部疾病严重危及患者生命安全,而颅脑手术是治疗该类疾病的最直接有效的方法,但风险极高、难度极


梅斯医学MedSci APP
医路相伴,成就大医
#硬膜下#
33
学习学习.不错的病例
59
学习
56
学习谢谢分享
58