Eur Radiol:蛋蛋长病了?动态增强和扩散加权MR成像在显示隐匿性实性小睾丸肿瘤的价值
2017-09-05 shaosai MedSci原创
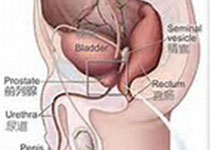
精原细胞瘤多发生于中年以后,常为单侧性,右侧略多于左侧。发生于隐睾的机率较正常位睾丸高几十倍。本瘤为低度恶性。85%的患者睾丸明显肿大,肿瘤局部侵犯力较低,肿瘤一般有明显界限。精原细胞瘤发展较慢,一般先转移至腹膜后淋巴结,后期也可发生广泛血道播散,确诊时,临床期病例占60%~80%。本研究旨在评价利用动态对比增强(DCE)磁共振成像(MRI)的半定量和定量指标以及扩散加权(DW)MRI在鉴别良恶性
精原细胞瘤多发生于中年以后,常为单侧性,右侧略多于左侧。发生于隐睾的机率较正常位睾丸高几十倍。本瘤为低度恶性。85%的患者睾丸明显肿大,肿瘤局部侵犯力较低,肿瘤一般有明显界限。精原细胞瘤发展较慢,一般先转移至腹膜后淋巴结,后期也可发生广泛血道播散,确诊时,临床期病例占60%~80%。本研究旨在评价利用动态对比增强(DCE)磁共振成像(MRI)的半定量和定量指标以及扩散加权(DW)MRI在鉴别良恶性隐匿性实性小睾丸肿瘤的价值,并将结果发表在Eur Radiol上。本研究共纳入了47例隐匿性实性小睾丸肿瘤的患者,并行DCE-MRI和DWI检查。计算肿瘤相关影像学参数及指标:增强峰度(PE)、达峰时间(TTP)、增强峰度百分比(Epeak)、流入速率(WIR)、强化信号比率(SER)、量转移常数(K trans)、速率常数(K ep)、血管外细胞外空间体积分数(Ve)和首次曲线下面积(iAUC)。评价DWI信号强度和表观弥散系数(ADC)。良性组E peak、WIR、K trans 、K ep 和iAUC 要高于恶性组,而TTP要低于恶性组(p<0.05)。所有肿瘤ADC值相似(p &
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#睾丸肿瘤#
31
#隐匿性#
32
#睾丸#
39
#隐匿#
33
学习了谢谢分享
52