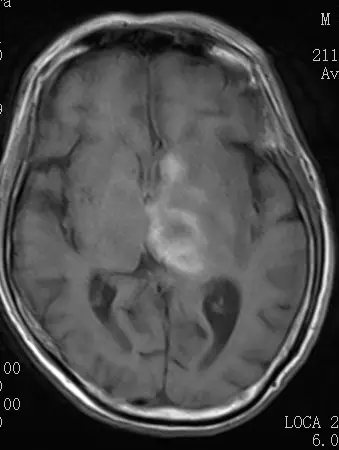
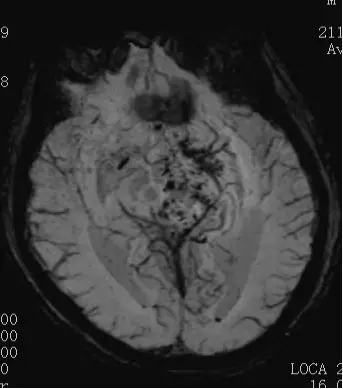
脑出血还用抗凝药物治疗,症状好转,什么情况?
2018-05-26 火眼金睛 医学界神经病学频道
患者,老年、女性,既往“上消化道肿瘤行手术治疗10余年一直复查随访未复发。本次因言语不清、右侧肢体无力进行性加重2天入院。


本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言


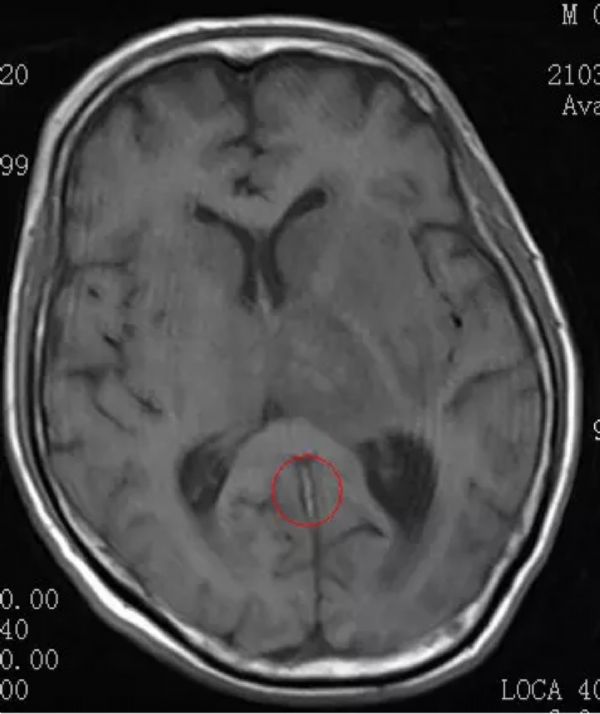

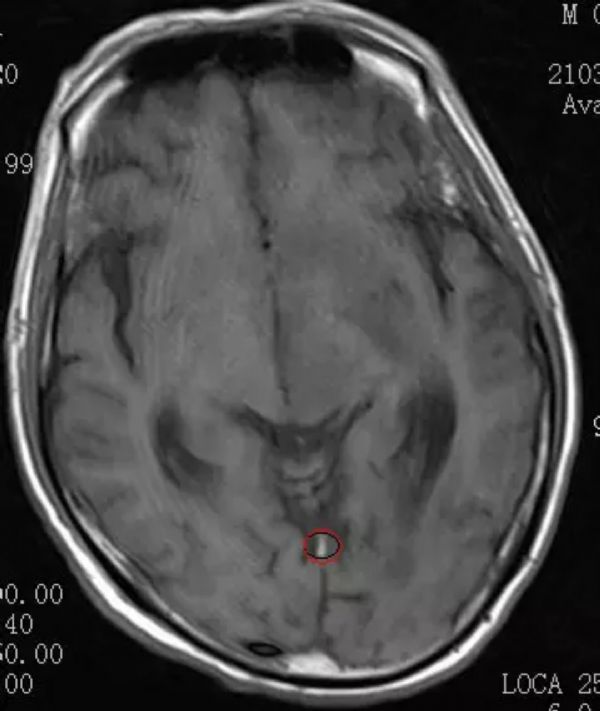
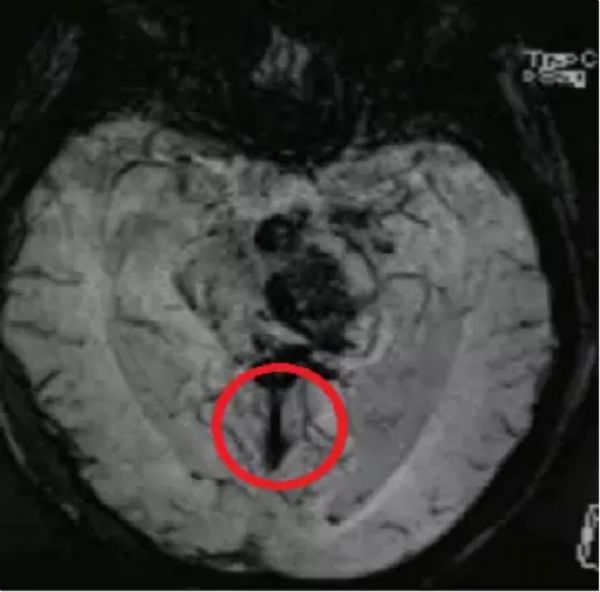
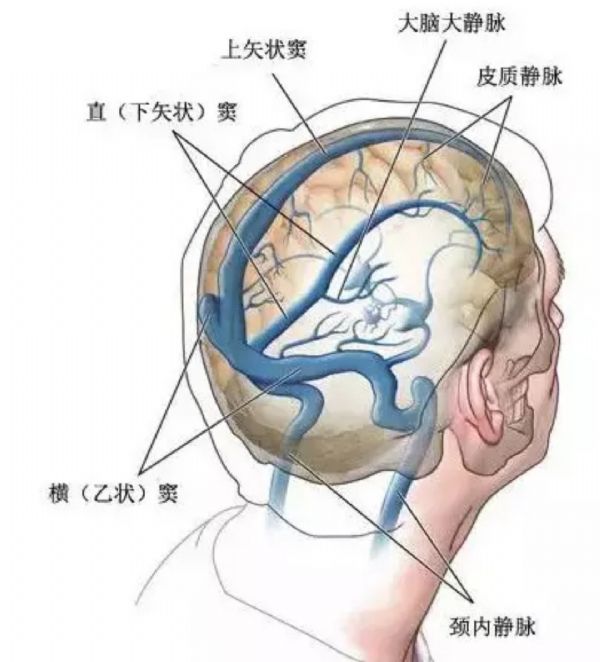











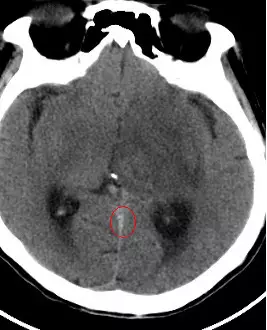
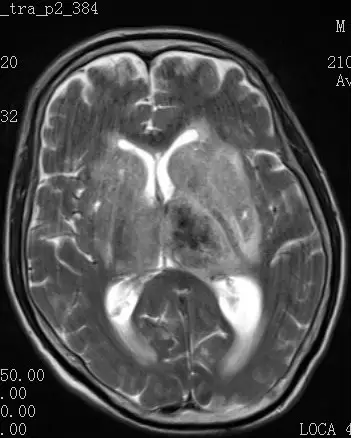
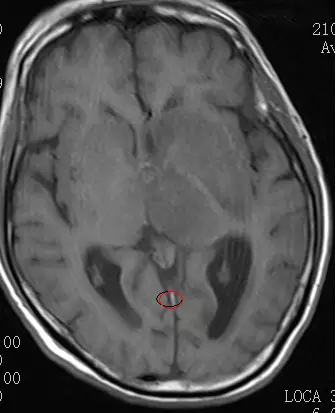
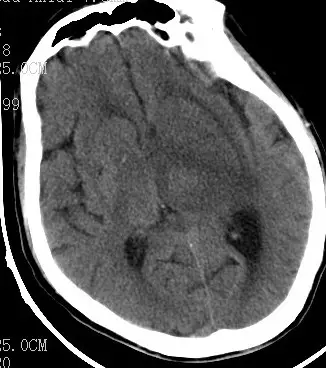
静脉窦血栓
67
这个影像学应该比较明确了
62
好文献学习了
52
学习了长知识
54
学习了长知识
61
学习了长知识
26
学习了长知识
29
好文献学习了
22
谢谢分享.学习了
28
学习学习.很好
26