临床症状难辨泌尿系结核与感染 如何才能避免误诊?
2018-08-10 尚云晓 薛辛东 儿科急重症与疑难病例诊治评述
12岁女童,因“间断低热、夜尿增多1个月”就诊,以“泌尿系感染”收治入院。超声提示,右肾及输尿管改变。同时CT显示,双肺上叶尖背部不均匀斑片状影。得知女童姐姐既往有肺结核病史,再综合其临床表现、化验检查结果及抗感染疗效,确定为肾结核可能性大。该病临床症状并不明显,为避免误诊漏诊,早期诊断需考察哪些方面?答案详见以下病例——
12岁女童,因“间断低热、夜尿增多1个月”就诊,以“泌尿系感染”收治入院。超声提示,右肾及输尿管改变。同时CT显示,双肺上叶尖背部不均匀斑片状影。得知女童姐姐既往有肺结核病史,再综合其临床表现、化验检查结果及抗感染疗效,确定为肾结核可能性大。该病临床症状并不明显,为避免误诊漏诊,早期诊断需考察哪些方面?答案详见以下病例——
【疾病概述】
肾结核(tuberculosis of kidney)是指结核分枝杆菌自肺部或其他器官结核灶经血行播散到肾脏引起的继发性感染。本病发病缓慢,早期无明显症状,严重者以顽固性尿路刺激症为主要临床表现,多见于20~40岁的中青年,男性发病多于女性,儿童罕见。约4%~9%肺结核可发生结构破坏的泌尿生殖系结核。
肾结核的主要原发病灶为肺结核,少数来自于骨、关节、肠、淋巴结的结核病灶。偶有从生殖道蔓延到肾脏。
肾脏结核的基本病理改变为结核结节或结核性肉芽肿形成。结核结节的中心为干酪样坏死组织,周围为类上皮细胞及朗汉斯巨细胞,外围为淋巴细胞及纤维组织。
结核分枝杆菌经血路侵入双肾,先在双侧肾脏的肾小球毛细血管丛中形成微结核病灶(病理性肾结核),在机体抵抗力正常的情况下,微结核病灶可痊愈或长期处于静止状态,不出现临床症状,但未痊愈的微结核病灶可引起结核菌尿。
初起病变是一个肾小球结核结节,以后可发生坏死性损害,并且蔓延到小管。大多数病例从隐匿到再活动10~40年,一旦形成干酪样坏死损害,极少能自愈。发生坏死性乳头炎到肾实质空洞形成、钙沉积;感染继续播散,肾盂炎症到纤维化,影响集合系统,形成狭窄和肾盂积水。如果实质纤维化进展,肾内血管狭窄,致纤维化,最终肾结构破坏。若“种植”到尿,可发生尿道炎、膀胱炎(伴有溃疡形成、纤维化及壁增厚)。
未进入临床肾结核阶段的患者,临床上无显著症状,但尿液结核菌可阳性。尿频、尿急、尿痛是肾结核的典型而突出的临床症状,尿频常最早出现,初发病时尿频可不伴尿痛,应用一般抗生素治疗无效。镜下有大量脓细胞,有时可发现坏死组织。严重的患者尿液可呈“米汤样”。肾结核局部症状不明显,压痛及肾肿块(积水)较少见。结核性脓肾继发感染(多数为大肠埃希杆菌)时,或肾周围寒性脓肿时可有局部叩压痛,甚至出现腰部窦道。严重患者或有其他器官结核时,可出现消瘦、乏力、潮热、盗汗、食欲减退。双肾功能严重障碍者可出现尿毒症。
约90%肾结核患者有蛋白尿、脓尿和血尿。无菌性脓尿应高度怀疑肾结核。除尿常规外,可连续数次做24小时浓缩尿直接涂片找抗酸杆菌,检查规范的实验室阳性率达70%。约90%患者结核分枝杆菌尿培养阳性。尿结核菌培养如阳性则可确诊泌尿系统结核。部分患者肾功能减退。90%有I VP异常、肾肿大、肾盏异常、“虫蚀形”溃疡。
如有肺结核史或有密切结核接触史,未接种过卡介苗者,有助于本病诊断。常需与非特异性尿路感染、肾肿瘤、肾结石等相鉴别。
肾结核是全身性疾病,要加强营养、改善生活环境、适当休息、合理的运动、保持良好的心态。不论是否需要手术治疗,所有患者都要先使用抗结核药物以控制结核的播散。抗结核药物问世之前,肾结核的治疗主要是切除感染的肾脏;抗结核药物广泛应用于肾结核之后,不仅可以治愈早中期患者,而且也显著改善了严重及晚期肾结核患者的预后,使需要外科手术治疗的患者大大减少,极大地保护了肾功能。早期治疗效果明显,晚期治疗预后不良。
【病例介绍】
患儿,女,12岁,因“间断低热1个月,尿常规异常1天”入院。其姐姐既往有肺结核病史。患儿近1个月间断低热,夜尿增多,排尿终末疼痛,无尿急,无腰部疼痛,无咳嗽咳痰,无盗汗,无疲倦乏力,饮食睡眠良好,就诊于我院门诊。查尿常规:蛋白(2+),白细胞321.03/HP,红细胞15.35/HP,以“泌尿系感染”收入我科诊治。入院查体:体温37.2℃,脉搏84次/分,呼吸20次/分,血压80/62mmHg,精神状态良好,体型消瘦,体重28kg(低于同年龄x─-2SD),身高1.41c m(低于同年龄x─-1SD),浅表淋巴结未触及肿大,心肺腹查体均正常,肾区无叩痛,膀胱区无压痛。
辅助检查:血常规:WBC6.5×109/L,N%64﹒7%,L%25﹒9%,HB126g/L,PLT312×1012/L。尿常规:蛋白(+),WBC364.75/HP,RBC10.30/HP,细菌计数正常。CRP:18.5mg/L。24小时尿蛋白定量0.88g。肾小管功能:尿转铁蛋白7.50mg/dl,尿微量蛋白68.0mg/dl,尿α1微球蛋白4.34mg/dl。PPD试验:d=0.8c m。淋巴细胞亚群:NK2,总B细胞25,总T细胞、Ts/Th正常。体液免疫、血沉、血清补体、肝肾功、心肌酶谱正常。血清结核抗体、血细菌培养、2次尿细菌培养均阴性。胸部X线平片:右肺尖少量纤维索条影。肺CT(图7‐1):双肺上叶尖背部不均匀斑片状影,右侧明显。泌尿系超声提示(图7‐2,见文后彩插):①符合双肾弥漫性损伤改变;②右肾积水;③慢性膀胱炎。静脉肾盂造影(I VP:图7‐3):顺利经静脉注入欧乃派克30ml,左侧肾盂肾盏输尿管充盈良好、形态正常,仰卧位上延长时间一直未见右侧尿路显影,膀胱充盈可,壁不光滑。逆行排泄性泌尿系造影:膀胱充盈,壁不光滑,未见输尿管反流,注意膀胱炎。I VP检查后1小时行双肾64层CT平扫+体层(三维)提示(图7‐4,见文后彩插):右肾及输尿管改变,需注意慢性肉芽肿性疾病的可能(结核?),右肾积水,排泄延迟,直肠前方右附件区钙化灶。肾小球滤过率:T‐GFR 60﹒21ml/min,R‐GFR6.66ml/min,右肾功能极重度改变;L‐GFR53.56ml/min,左肾GFR正常,左肾功能正常。予患儿头孢吡肟抗感染治疗8天后,效果不理想。尿常规:蛋白(+2),WBC24.79/HP,RBC2.21/HP,细菌计数正常。CRP13.20mg/L。综合患儿临床表现、化验检查结果及抗感染疗效,考虑结核病可能性大,请沈阳市结核病院专家会诊协助诊断为双肺结核、肾结核、输尿管膀胱结核、右附件结核,转入沈阳市结核病院进一步治疗。
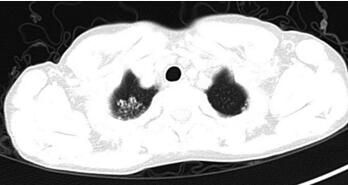
图7‐1 肺CT:原发结核病灶

图7‐2 泌尿系彩超:双肾实质回声普遍增强,皮髓质界限模糊,未见占位性病变;右肾大小约10.9cm×4.8cm,肾盂肾盏扩张,壁增厚,以肾盏扩张明显,右输尿管全程扩张,上段直径约0.7c m,下段直径约0.6cm;左肾大小约10.8cm×3.7cm,左输尿管未见扩张,膀胱充盈良好,内壁不规整增厚,较厚处约0.5cm,回声粗糙,未见占位病变

图7‐3 IVP:左侧肾盂肾盏输尿管充盈良好,形态正常,仰卧位上延长时间一直未见右侧肾盂肾盏显影
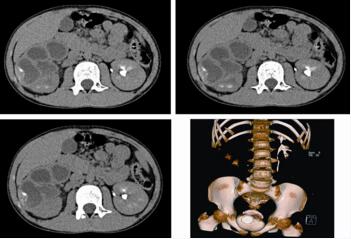
图7‐4 双肾CT:右肾体积明显增大,皮质变薄,实质内多发囊状低密度影,呈“花瓣样”围绕肾盂排列,肾盏明显增宽,其内可见少量造影剂排泄影及液液平,盂管交界部及输尿管管壁增厚,右侧输尿管内见造影剂。左肾大小形态未见异常,肾盂肾盏未见扩张,左侧输尿管不宽,可见造影剂填充,膀胱充盈可,壁不光滑,直肠前方右附件区见结节样高密度灶,肠管走行自然,未见管壁增厚
【诊断评述】
1﹒儿童泌尿系结核临床症状与泌尿系感染区别不大,如果难治性泌尿系感染或反复发作,临床应注意泌尿系结核的可能。结核病的中毒症状在肾结核并不明显,易误诊漏诊。
2﹒儿童泌尿系结核发病率低,一般在肺结核的基础上5~25年可能发展为儿童泌尿系结核。
3﹒泌尿系结核的早期诊断不能单纯依靠临床症状,实验室检查是临床诊断泌尿系结核的重要手段,应综合分析各项化验检查结果。尿液检查在早期诊断泌尿系结核中占重要地位,结核菌常间断排出,故尿结核分枝杆菌培养应连续检查3~5次为宜。但血与尿结核分枝杆菌培养阴性、血清结核抗体阴性并不能排除结核病。血沉正常亦不能排除活动性结核。
4﹒影像学检查是泌尿系结核诊断的关键,对I VP显影差或不显影的患儿,CT检查的实用价值更大,能清楚显示肾脏形态、扩大的肾盏和肾盂以及空洞、积液、钙化等表现,应作为肾结核的首选影像学检查方法。IBD%E8%AF%8A%E6%B2%BB%E8%BF%87%E7%A8%8B%E4%B8%AD%E7%9A%84%E8%AF%84%E4%BC%B0-Part%204" target="_blank">B超检查可能仅提示肾脏大小、肾积水或囊肿样改变。
5﹒鉴别诊断应注意:①多囊肾:囊肿数目更多且散在分布,囊壁光滑,钙化几率低,一般不累及肾盏、输尿管,常合并其他部位多发囊肿;②非结核性积水:肾盂肾盏均匀扩张,与实质分界清晰,肾外形多匀称性肿大,肾盂输尿管壁无增厚;③黄色肉芽肿性肾盂肾炎:一般由肾和(或)输尿管结石致肾盏颈部或肾盂输尿管交界处狭窄积水,继发非特异性感染,尿培养几乎总是阳性,临床常有类似结核病的表现;④肾盂肾炎:其与肾结核的临床表现极为相似,两者可均有腰痛、尿路刺激症状、镜下或肉眼血尿、白细胞明显升高时可有蛋白尿,肾盂肾炎可有高热,抗生素治疗效果较好;⑤慢性膀胱炎。
【临床经验】
1﹒儿童泌尿系结核发生发展过程隐匿,临床表现多不典型,症状可以很轻微或间断发作,同时伴有尿路刺激症状、腰痛及血尿等典型症状的病例并不多见,常易忽视,能否早期诊断,有赖于临床医生的警惕性。
2﹒应重视儿童泌尿系感染的影像学诊断,如果临床泌尿系感染诊断不确切,肾功能允许的条件下应尽早做静脉泌尿系造影或泌尿系增强CT,以早期诊断一些泌尿系的少见疾病。
3﹒对于有肺结核或有确切结核接触史的患儿,应监测尿常规以早期发现异常。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#临床症状#
31
认真观察,仔细思考
61
#结核#
41
#泌尿系#
25
很好的病例
52
学习了谢谢分享
51