医患有必要成为朋友吗?
2017-10-16 佚名 医学生
如今,医患之间的关系逐渐变得紧张,让医患成为朋友是一个愿景也是大家期待的事情。但就事实而言,医生与患者大可不必成为朋友。
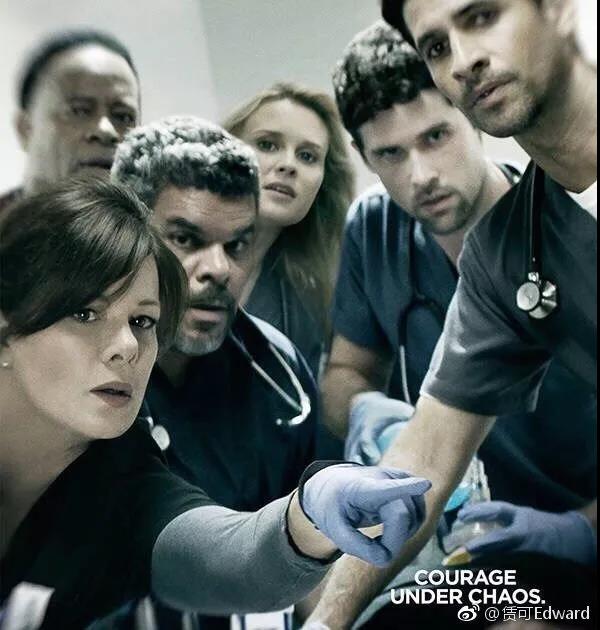
如今,医患之间的关系逐渐变得紧张,让医患成为朋友是一个愿景也是大家期待的事情。但就事实而言,医生与患者大可不必成为朋友。医生的特殊性 越熟越不易诊疗不必是因为关心则乱。做为医生都能知道,越是熟人越容易出岔头。一边是医生想多快好省地解决问题,一边是患者把医生朋友当救命稻草,盲目信任,有话不明说,事后猜忌。于是,筋疲力尽地好心办坏事,认认真真地费力不讨好,不胜枚举。和医生的关系越密切,就能得到越好的治疗吗?肯定不是的。一旦有了医患之外的交情后,会影响医生对病情和治病方案的判断和决定。有个老教授深静脉血栓,老教授的夫人是著名的血液内科教授,参与会诊讨论的时候,竟然拿不出抗凝治疗的意见。原因是她太了解利弊了。至亲的身份让她乱了阵脚,在利弊之间左右为难,难以定夺。就是这样,医生确实能够更加了解治疗方案的利弊,但是由于感情因素的参杂,倒不如置身其外,能够冷静的选择方案。医生每日都会应接不暇的接待患者,倘若都成为朋友,压力也会很大。人们都希望有个医生朋友。病人们也有时会想跟医生成为朋友,出发点不尽相同。有的是希望今后多个朋友多条路。自己的病需要定期随诊,家人出了健康状况也需要有个人咨询。你看我也拥有
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习了
37
不能掺杂
40
#医患#
17
没有必要主动拉进关系
37
有时确实是这样
42
学习了新知识
36
生命所托.医生
25
谢谢分享.学习了
24
好好学习天天学习
28
没有必要吧!
21