EBioMedicine:科学家发现决定是否过敏的基因!过敏疫苗或指日可待!
2018-04-23 佚名 “细胞”微信号
你是否会发生过敏在很大程度上依赖于基因,这是一项最近发表在《EBioMedicine》上的新研究的主要结论。这项研究由维也纳医科大学免疫学研究所Winfried F. Pickl教授领导完成。他们发现HLA-DR1基因和过敏原特异性的反应性T细胞在针对艾蒿类植物的过敏中发挥着关键作用。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CIN#
19
#DIC#
22
#Bio#
14
#EBI#
25
#科学家发现#
30
#Medicine#
18
#Med#
21
标题党
62
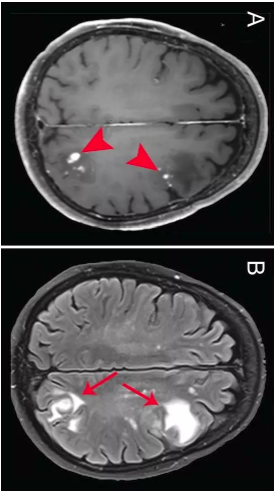
长期以来科学家都认为HLA分子在自身免疫性疾病.慢**染和过敏中发挥关键作用.在这项研究中.研究人员首次发现在四种小鼠模型中.只有携带HLA-DR1才会对艾蒿发生过敏.且需要过敏原特异性的活性反应性T细胞数量超过调节性T细胞.[结果就是哮喘爆发性的发作和致病性.过敏性特异性免疫球蛋白E的形成."Pickl解释道.艾蒿通过呼吸道引入.就和人们通常接触的一样.
56
这是一个有趣的研究
44