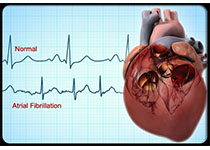
JAHA:增加的循环成纤维细胞是左心房纤维化和房颤复发的标志!
2018-03-13 xing.T MedSci原创
由此可见,在持续性房颤患者中,增加的循环成纤维细胞可以作为LA纤维化与房颤复发的标志。
在心房颤动(AF)患者中,更广泛的纤维化左心房(LA)提供了心律失常的基础,并增加射频消融后复发的风险。成纤维细胞是骨髓来源的循环间充质细胞,已在有心脏瓣膜疾病的AF的患者心房中得到了鉴定。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究旨在探讨持续性房颤患者消融后循环成纤维细胞与LA纤维化或复发率之间的相关性。
研究人员测量了来自于持续性房颤患者(n=40)、阵发性房颤患者(n=30)以及窦性心律对照者(n=30)循环成纤维细胞的比例、分化和迁移水平。LA低‐电压(纤维化)区域是通过电解剖标测系统来进行鉴定,并在射频消融后随访1年。研究人员采用多元回归分析评估循环纤维细胞百分比与LA低电压区域或复发之间的相关性。
研究人员发现在在持续性房颤患者中循环纤维细胞百分比与LA低电压面积呈正相关,循环纤维细胞(≥4.05%)是消融后1年内复发的显著预测因子。在持续性房颤组(67.58±1.54%)相比于阵发性房颤组(56.67±1.52%)和窦性心律组(48.43±1.79%)培养的成纤维细胞表现出增强的分化潜能。此外,在持续性房颤患者分化的成纤维细胞中成纤维细胞活化和细胞迁移能力的标志物表达也升高。转化生长因子β1和基质细胞衍生因子-1在持续性房颤患者的血浆中升高,被证明分别可以促进成纤维细胞的分化和迁移。
由此可见,在持续性房颤患者中,增加的循环成纤维细胞可以作为LA纤维化与房颤复发的标志。
原始出处:
Yang Liu,et al. Elevated Circulating Fibrocytes Is a Marker of Left Atrial Fibrosis and Recurrence of Persistent Atrial Fibrillation, JAHA.2018. https://doi.org/10.1161/JAHA.117.008083
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#左心房#
57
#AHA#
29
#成纤维细胞#
42
#纤维细胞#
35
#心房#
36
学习一下谢谢
61
学习了
60