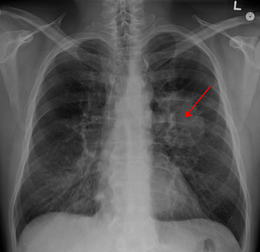
J Clin Oncol:局部晚期非小细胞肺癌:强度调控放疗vs三维适形体外放疗
2017-04-13 选题审校:韩茹 编辑:吴星 环球医学编译
专家点评:IMRT被定义为在放疗过程中,改变能量频率和随后的放疗剂量。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Oncol#
24
#局部晚期#
34
#非小细胞#
30
文章不错,拜读了
61
感谢小编为我们精心准备了如此精辟的精神大餐,小编辛苦了!
70
#局部#
27