Eur Arch Otorhinolaryngol:在过敏性鼻炎儿童中,白介素-33能够促进辅助T细胞类型-2/17炎症反应
2017-11-29 AlexYang MedSci原创
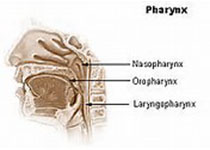
白介素-33是最近才被描述的细胞激素,并且与辅助T细胞类型2(Th2)调控的疾病有关。然而,它在儿童过敏性鼻炎(AR)发病机理中的调控角色仍旧需要进一步的鉴定。最近,有研究人员进行了旨在评估IL-33在患有AR儿童中的表达情况以及作用。研究包括了40名患有AR的儿童,并且还包括了20名健康的对照,并通过酶联免疫反应试验(ELISA)分别检测了IL-33和Th细胞激素在血清和鼻腔灌洗液中的产生情况。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞类型#
30
#过敏性#
37
#辅助T细胞#
26
#炎症反应#
34
#白介素#
25
学习了谢谢分享
56
学习了
38
学了......
58
学习一下谢谢
49
学习
53