BMB Rep:人羊膜来源间充质干细胞通过ERK1/2 MAPK信号通路诱导人脂肪干细胞的成骨和血管生成
2018-03-16 MedSci MedSci原创
间充质干细胞(MSCs)在治疗骨缺损方面显示出巨大的潜力。人类脂肪干细胞(HASCs)是具有多谱系分化潜能的多能祖细胞。人羊膜来源的间充质干细胞(HAMSCs)能够促进MSCs的成骨分化。 在这项研究中,我们通过transwell共培养系统研究了HAMSCs对HASCs的影响。结果显示,HAMSCs可促进HASCs的增殖、成骨分化、血管生成潜能和脂联素(APN)分泌。此外,U0126是一种高选择性
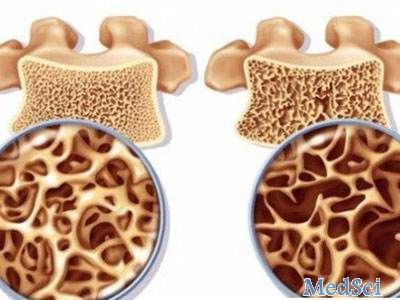
间充质干细胞(MSCs)在治疗骨缺损方面显示出巨大的潜力。人类脂肪干细胞(HASCs)是具有多谱系分化潜能的多能祖细胞。人羊膜来源的间充质干细胞(HAMSCs)能够促进MSCs的成骨分化。
在这项研究中,我们通过transwell共培养系统研究了HAMSCs对HASCs的影响。结果显示,HAMSCs可促进HASCs的增殖、成骨分化、血管生成潜能和脂联素(APN)分泌。此外,U0126是一种高选择性细胞外信号调节激酶1/2(ERK1/2)丝裂原活化蛋白激酶(MAPK)信号通路抑制剂,可显著抑制HAMSCs的积极作用。
综上所述,该研究结果表明HAMSCs通过ERK1/2MAPK信号通路诱导HASCs中的骨再生。
原始出处:
Wang Y, Chen X, et al., Human amnion-derived mesenchymal stem cells induced osteogenesis and angiogenesis in human adipose-derived stem cells via ERK1/2 MAPK signaling pathway. BMB Rep. 2018 Feb 12. pii: 4075. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#MAPK#
39
#间充质干细#
36
#ERK#
25
#成骨#
20
#脂肪干细胞#
28
#信号通路#
21