Ann Oncol: 前列腺癌患者年龄相关的黄斑变性风险
2017-10-02 AlexYang MedSci原创
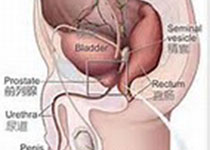
前列腺癌(PC)与增加的系统性的氧化胁迫和二氢睾酮水平相关,同样,之前也有报道表明了前列腺癌参与了年龄相关的黄斑变性(AMD)病理过程。最近,有研究人员进行了一项群体试验从而确定是否患有PC 的病人具有增加的AMD风险。研究人员从台湾地区纵向医疗保险数据库中搜集了1999年到2010年期间的数据资料。研究PC群体包括了22084名年龄不小于18岁且为首次诊断为PC的病人。对照组病人在年龄、职业和城
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#年龄相关#
25
#Oncol#
25
#变性#
38
#黄斑#
33
henhao
51
学习了受益匪浅
63