AHA 2017:杨跃进研究团队:中国ST段抬高AMI相关心源性休克的新近进展
2017-11-22 佚名 国际循环
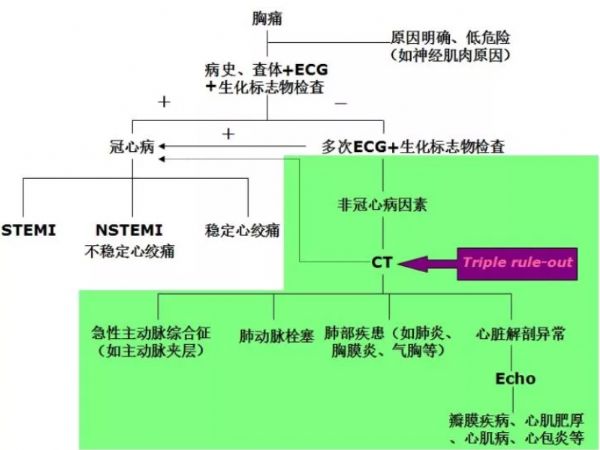
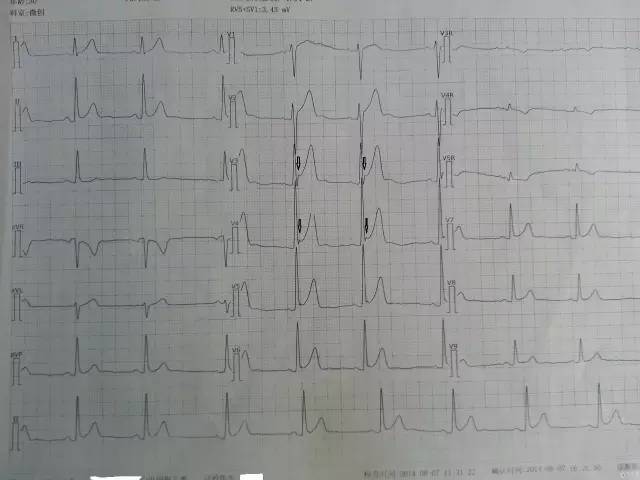
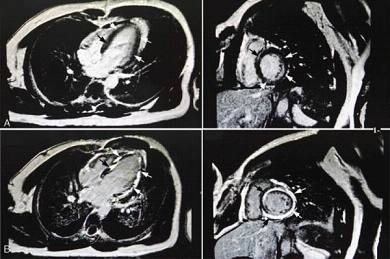
心源性休克大部分由心肌梗死引起,数据显示,6%~8%的ST段抬高型心肌梗死(STEMI)患者可发生心源性休克,是导致死亡的最主要原因。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









学习了.谢谢作者分享!
77
#AHA#
29
#心源性休克#
31
#ST段抬高#
30
#研究团队#
39
#心源性#
27
#ST段#
26
学习.谢谢分享
65
加强宣传.早期血运重建.改善预后
67