BMC Cancer:患者来源胃癌异种移植是一种有效的靶向治疗的临床前评价工具
2017-03-28 MedSci MedSci原创
靶向治疗是胃癌(GC)的新兴治疗方案。患者来源的肿瘤异种移植物(PDX)模型GC保留了原始临床癌症的特征,为临床前药物疗效测试提供了强大的工具。该研究旨在建立PDX GC模型,并探索靶向Her2,MET(cMet)和FGFR2的治疗方法,这可能有助于医生为选定的患者选择适当的靶向治疗。
近日,来自浙江大学医学院附属第一医院的研究人员通过构建人源化肿瘤异种移植模型进行了胃癌靶向药物筛选,相关研究成果刊登于国际杂志BMC Cancer上,该研究为开发新的胃癌靶向治疗药物提供了重要信息。
靶向治疗是胃癌(GC)的新兴治疗方案。患者来源的肿瘤异种移植物(PDX)模型GC保留了原始临床癌症的特征,为临床前药物疗效测试提供了强大的工具。该研究旨在建立PDX GC模型,并探索靶向Her2,MET(cMet)和FGFR2的治疗方法,这可能有助于医生为选定的患者选择适当的靶向治疗。
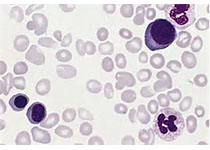
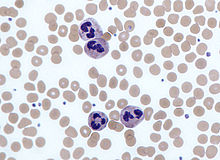
研究人员收集了32名病人的胃癌组织,移植到免疫缺陷小鼠体内,并借助多种实验技术对Her2,cMet和FGFR2的表达水平进行了评估。最后利用构建的PDX模型检测靶向抑制剂的抗肿瘤效果。
研究表明,这些PDX GC模型为药物筛选和评估提供了理想的平台。具有阳性cMet或FGFR2基因扩增的GC患者可能潜在地受益于cMet或FGFR2靶向治疗或组合靶向治疗。
原始出处:
Haiyong Wang†, Jun Lu†, Jian Tang, Shitu
Chen. et al. Establishment of patient-derived gastric cancer xenografts: a
useful tool for preclinical evaluation of targeted therapies involving
alterations in HER-2, MET and FGFR2 signaling pathways. BMC Cancer201717:191 DOI:
10.1186/s12885-017-3177-9
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#BMC#
33
靶向治疗是个趋势
89
感谢分享一下!
90
#评价#
31