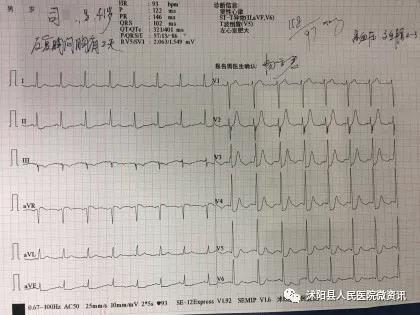
Circulation:高灵敏度心肌肌钙蛋白I与肌钙蛋白T联合应用于急性心肌梗死的早期诊断
2018-09-16 MedSci MedSci原创
结合心肌细胞损伤的两种信号,心肌肌钙蛋白I(cTnI)和T(cTnT),或许可仅采用抽血来克服个别病理生理学和分析的局限性,从而提高对急性心肌梗死的诊断准确性。现研究人员对采用高敏感(hs)cTnI和hs-cTnT联合用于急性心肌梗死的早期诊断价值进行评估。与单独应用相比,hs-cTnI和hs-cTnT联合使用并不能持续提高总体诊断的准确性。但是,联合应用可提高符合早期排除标准的患者比例。根据欧洲
与单独应用相比,hs-cTnI和hs-cTnT联合使用并不能持续提高总体诊断的准确性。但是,联合应用可提高符合早期排除标准的患者比例。根据欧洲心心脏病学会2015年指南推荐的算法和界限,基线采血后,符合排除标准的患者比例有限(6%-24%)。采用hs-cTnI和hs-cTnT浓度之和(9ng/L)和乘积(18ng2/L2)为合理的排除标准可将原队列单次采血后符合排除标准的患者比例升高至34%-41%(和:阴性预测值[NPV]100%[95% CI 99.5%-100%];积:NPV 100%[95% CI 99.5%-100%),在验证队列中,(和:NPV 99.6%[95% CI 99.0-99.9%];积:NPV 99.4%[95% CI 98.8-99.8%])。采用联合算法(hs-cTnI<4ng/L和hs-cTnT<9ng/L)显示排除率(40%-43%,NPV原始队列99.9%[95% CI 99.2-100%];NPV 验证队列 99.9%[95% CI 98.9-99.8%)和纳入率(阳性预测值[PPV]原始队列74.4%[95% CI 69.6-78.8%];PPV 验证队列84.0%[95% CI 79.7-87.6%])结果相似。
结合hs-cTnI和hs-cTnT浓度的新方法可明显增加符合极早期安全排除条件的患者数量,但对明确急性心肌梗死似乎没有什么帮助。
Noreen van der Linden,et al.Combining High-Sensitivity Cardiac Troponin I and Cardiac Troponin T in the Early Diagnosis of Acute Myocardial Infarction. 24 Apr 2018.Circulation. 2018;138:989–999
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#灵敏度#
49
#联合应用#
46
#早期诊断#
49
#心肌肌钙蛋白#
48
#肌钙蛋白T#
40
#肌钙蛋白I#
38
有用
68
了解一下,谢谢分享!
69