EuroPCR2018丨Tryton支架系统与临时支架治疗真性分叉病变的结局对此
2018-05-27 国际循环编辑部 国际循环
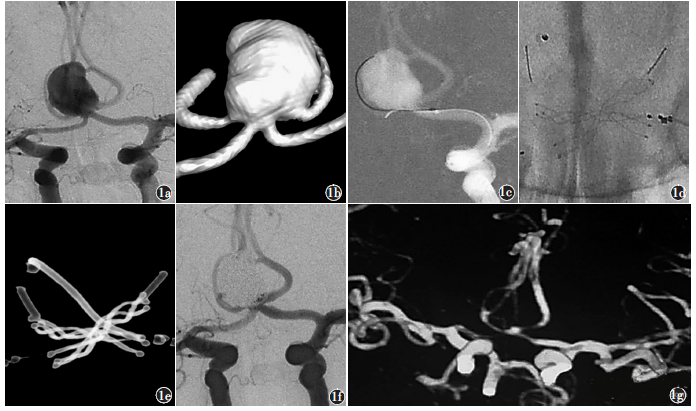
分叉病变的手术成功率较低,不良心血管事件风险较高。目前,临时支架(PS)是治疗分叉病变的默认方法,Tryton支架是治疗真性分叉病变的专用分叉支架系统。EuroPCR 2018大会,纽约心血管研究基金会KONIGSTEIN M.等研究者开展的一项研究,旨在评估采用Tryton支架系统治疗涉及大分支(SB)的真性分叉病变的安全性及有效性。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#EuroPCR#
42
#支架治疗#
56
#PCR#
31
#分叉病变#
64
学习学习学习
0
不错的文章值得推荐一下
59
不错的文章值得拥有
59
了解一下.谢谢分享!
54
学习一下谢谢
69