赵明威教授丨抗VEGF时代糖尿病视网膜病变诊疗策略
2019-09-06 Fiona MedSci原创
在糖尿病视网膜病变的治疗中,抗VEGF药物治疗的应用越来越广泛。但是,在临床治疗中也存在误区,如果用好抗VEGF药物呢?在2015年公布于美国ARVO会议的RISE RIDE研究结果表明,抗VEGF可“逆转”糖尿病视网膜病变病程。经抗VEGF治疗1年后,约30%的患者严重程度较基线改善,微血管瘤、渗出、新生血管等病变有一定程度吸收和减少。但是,这只是治标不治本,并未改善病源根基。像视网膜毛细血管周
在2015年公布于美国ARVO会议的RISE RIDE研究结果表明,抗VEGF可“逆转”糖尿病视网膜病变病程。经抗VEGF治疗1年后,约30%的患者严重程度较基线改善,微血管瘤、渗出、新生血管等病变有一定程度吸收和减少。但是,这只是治标不治本,并未改善病源根基。像视网膜毛细血管周细胞凋亡、内皮细胞增值、毛细血管闭锁等DR的基础病例并未发生改变!
因此,RISE RIDE研究结论不能表述为“逆转”。
该研究的局限性在于,是在DME人群中以视力指标为首要目标的RCT研究,不是以DR的等级变化为主要终点的临床试验。未来还需以DR改善为主要终点的研究进一步验证抗VEGF在 治疗DR方面的疗效以及具体给药方式。
那么,抗VEGF治疗能否取代PRP治疗糖尿病视网膜病变?
虽然PRP有效,但并不完美。对于糖尿病患者来说,随着病程进展,会出现周边视力或视野丧失、暗视力减少或丧失、阅读能力减退和激发黄斑水肿导致的中心视力丧失。
在抗VEGF和全视网膜光凝两种治疗方法在周边视野损失的比较中,在2年时全视网膜光凝组比抗VEGF组视野缺损(从基线计算)明显,但在2-5年,两组周边视野的损失都在进展,到5年末没有差别,这也就意味着,抗VEGF组的视野缺损显著提速。
这种抗VEGF治疗的副作用,到底是因为启动了细胞凋亡通路,还是加快了糖尿病神经元病变?目前原因还在研究中。
全视网膜光凝(PRP)的原理为,光凝处耗氧高的视细胞为耗氧低的癫痕替代,视网变薄,脉络膜氧供视网膜内层,改善视网膜缺氧状态,维持正常的氧张力,牺牲周边视力,保全中心视力。
因此,赵明威教授强调, PRP是增值性糖尿病视网膜病变的根本治疗!
高危PDR是指≥1/4视盘面积的视盘新生血管,伴有玻璃体腔积血的任何视盘新生血管,伴有≥1/2视盘面积视网膜新生血管的玻璃体积血或视网膜前出血。
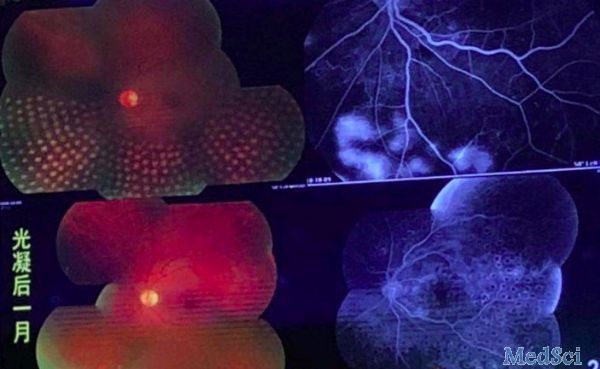
赵明威教授认为,抗VEGF疗法是糖尿病黄斑水肿的首选治疗方法,PRP是增殖性糖尿病视网膜病变的根本治疗。对于高危PDR,抗VEGF疗法应作为辅助治疗。可以先使用抗VEGF治疗抑制新生血管,在药物作用有效期内完成PRP,可以避免因为PRP起效慢而导致的病情进展,例如在尚未完成PRP时发生玻璃体出血甚至发生NVG。
最后,赵明威教授用一首诗总结道:
积极主动治“新青”,
力降眼压保视明,
先抗血管后手术,
成功关键在光凝。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#视网膜#
39
#VEGF#
32
#视网膜病变#
29
#抗VEGF#
37
谢谢MedSci提供最新的资讯
45