JACC:接受SAVR和经股动脉TAVR治疗的患者1年后的结果相似
2015-08-11 崔倩 译 MedSci原创
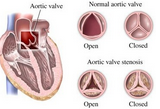
在真实环境中,目前对于经导管主动脉瓣置入术(Transcatheter Aortic Valve Implantation,TAVR)与外科主动脉瓣置入术(Surgery Aortic Valve Replacement,SAVR)的前瞻性和对照性的数据比较少。该研究的目的是描述接受SAVR和经股动脉TAVR的一系列倾向匹配患者1年的临床结果。这项OBSERVANT(对于严重主动脉瓣狭窄
在真实环境中,目前对于经导管主动脉瓣置入术(Transcatheter Aortic Valve Implantation,TAVR)与外科主动脉瓣置入术(Surgery Aortic Valve Replacement,SAVR)的前瞻性和对照性的数据比较少。
该研究的目的是描述接受SAVR和经股动脉TAVR的一系列倾向匹配患者1年的临床结果。
这项OBSERVANT(对于严重主动脉瓣狭窄治疗的SAVR-TAVI治疗有效性的观察研究)试验是一个前瞻性多中心观察性队列研究,参与的患者为主动脉瓣狭窄(AS)并接受SAVR或TAVR治疗的患者。应用该倾向得分的方法来选择2组基线特征相似的患者。所有的结果都通过与管理数据库的链接进行分析。这一分析的主要终点为在1年时任何原因和主要不良心脏和脑血管事件(MACCE)引起的死亡。
未经调整的招募的人群(n=7618)包括5,707例SAVR患者和1,911例TAVR患者。匹配的人群共有1300例名患者(每组650例)。倾向得分方法生成了一组低-中危险人群(平均logistic EuroSCORE 1:10.2±9.2% vs 9.5±7.1%,SAVR vs 经股动脉TAVR;P=0.104)。在1年时,全因死亡率手术组为13.6%,导管组为13.8%(风险比[HR]:0.99;95%置信区间[Cl]:0.72〜1.35;P =0.936)。同样的,两组的MACCE的发生率无显著差异,手术组和导管组分别为17.6%和18.2%(HR:1.03;95%Cl:0.78〜1.36;P=0.831)。在1年时脑血管事件和因心脏原因再住院以及急性心脏衰竭的累积发生率在两组是相似的。
结果表明,SAVR和经股动脉TAVR在1年时有相似的死亡率,不良心脏和脑血管事件,和由于心脏原因再住院率。这些数据需要在更长期和持续的随机试验中得到证实。
原始出处:
Corrado Tamburino, MD∗; Marco Barbanti, MD∗; Paola D’Errigo, RS‡; Marco Ranucci, MD§; Francesco Onorati, MD‖; Remo Daniel Covello, MD¶; Francesco Santini, MD#; Stefano Rosato, RS§; Gennaro Santoro, MD∗∗; Danilo Fusco, RS††; Claudio Grossi, MD‡‡; Fulvia Seccareccia, RS‡,1-Year Outcomes After Transfemoral Transcatheter or Surgical Aortic Valve Replacement,JACC,2015.8.11
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#经股动脉#
28
#AVR#
25
#JACC#
36
#股动脉#
38
外科的事越做越少啊
53
#ACC#
24
#SAVR#
36
有意思,但是tavr的入选标准很严格,如果结局跟savr一样就是了不起的进展
102